Updated on August 6, 2024
While there will always be an element of unpredictability with any form of cancer, people who are diagnosed with early-stage breast cancer generally have a much better prognosis than people who are diagnosed with cancer that has progressed to later stages.
While breast cancer staging is complex and takes into account many factors about a particular cancer, early-stage refers to breast cancers that have not spread beyond the breast. This is also sometimes referred to as a localized stage.
Routine screenings for breast cancer are the key to early detection.
Mammograms and mortality rates
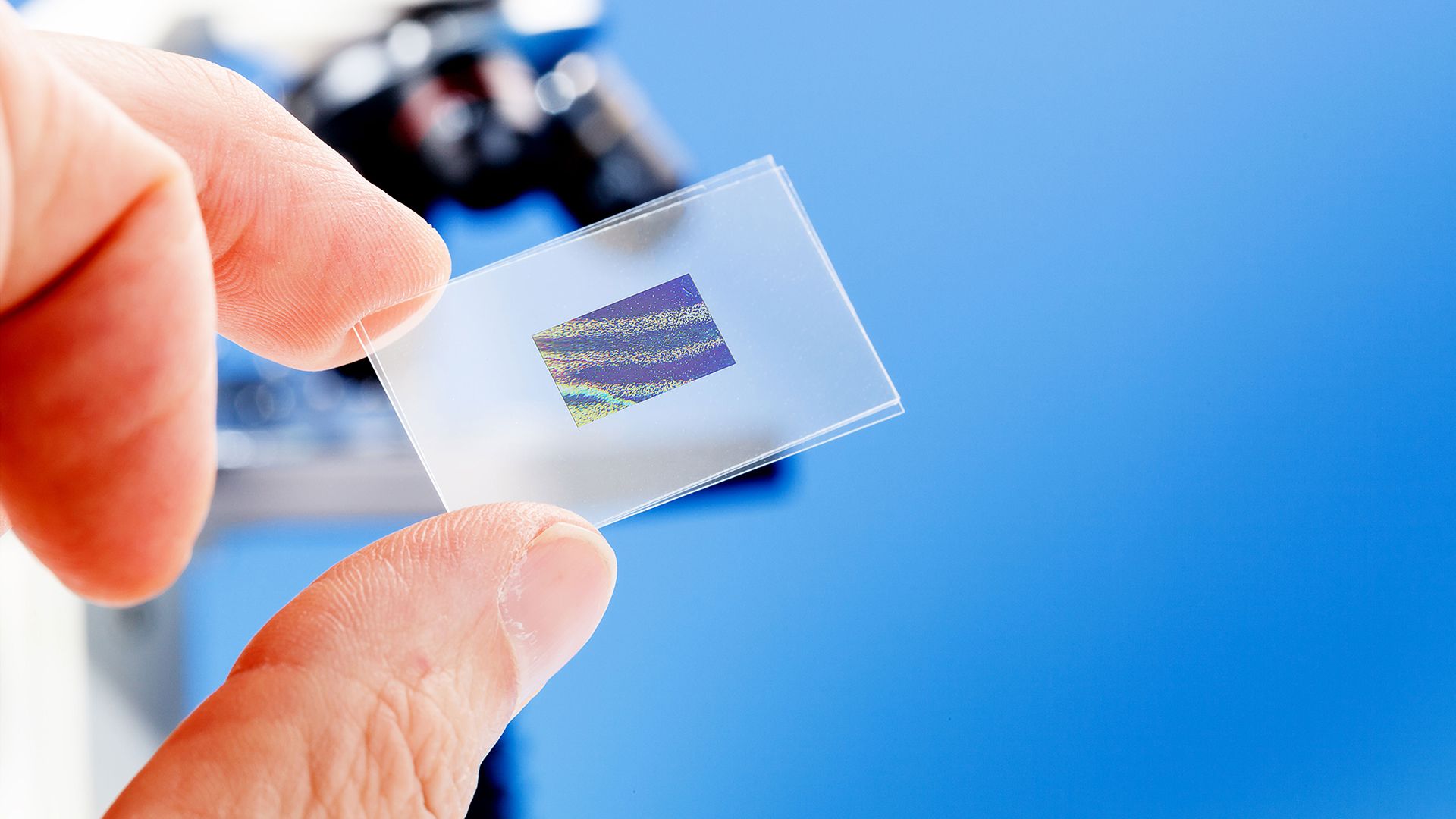
The standard for breast cancer screenings is an exam called a mammogram or mammography. During this exam, a breast is pressed between two plates of glass and an x-ray of the breast is taken. The x-ray provides an image of the inner structure of the breast tissue, including any abnormalities.
Multiple studies have found that women who attend mammography screenings have a much lower risk of dying from breast cancer. The conclusion is that more cancers are discovered earlier, before a cancer has spread and become more difficult to treat.
Mammography screenings at earlier ages are also cited as one of the ways to lower mortality rates among Black women with breast cancer in the United States.
When compared with all racial and ethnic groups in the U.S., Black women have the highest breast cancer mortality rate. This means that a greater percentage of Black women with breast cancer die as a result of having breast cancer. Compared with white women, for example, the mortality rate for Black women is about 40 percent higher.
Why are mortality rates higher?
There are multiple factors that are believed to contribute to the higher mortality rate among Black women with breast cancer. Many of these factors have to do with access to care, including screenings.
- Black women are much more likely to have triple-negative breast cancer (TNBC), an aggressive form of the disease that is more difficult to treat. Black women are also more likely to have comorbid conditions (such as hypertension, obesity, and diabetes) which can make TNBC more difficult to treat.
- While the incidence of breast cancer is lower among Black women, it is higher in Black women under the age of 60. Breast cancer may be more aggressive and less responsive to treatment in younger women.
- Some research shows that Black women who are diagnosed with breast cancer are less likely to have genetic testing for BRCA mutations. Identifying these mutations can help predict what cancer therapies will be most effective.
- Black women are less likely to be diagnosed at the localized stage and more likely to be diagnosed with a cancer that has spread beyond the breast.
When should you start screening?
Recommendations on when to begin screening for breast cancer vary depending on the organization that is publishing the guidelines.
Some organizations recommend that Black women should begin screening at age 40. Others argue that Black women should be added to the high-risk group due to the factors mentioned above, and they should begin talking to a healthcare provider about breast cancer risk no later than age 30.
Breast cancer screenings starting at age 40 are covered by most insurance plans, including government insurance programs like Medicare and Medicaid (though what is covered can vary from state to state).
People without insurance may be able to access no-cost cancer screenings through the National Breast and Cervical Cancer Early Detection Program (NBCCEDP).