Got back pain? These conditions may be to blame
Weren’t involved in an accident? Didn't lift anything heavy? Here are some other possible culprits.

Back pain is common. In fact, 8 out of 10 people in the United States experience it at some point in their lives. Back pain can result from injuries sustained during a fall or accident. Even some everyday habits, such as too much sitting, slouching or staring down at a screen can leave your back feeling stiff, achy or sore. But back pain could also be the result of an… Show More
Back pain is common. In fact, 8 out of 10 people in the United States experience it at some point in their lives. Back pain can result from injuries sustained during a fall or accident. Even some everyday habits, such as too much sitting, slouching or staring down at a screen can leave your back feeling stiff, achy or sore. But back pain could also be the result of an underlying medical condition.
It’s important to understand what’s causing your back pain and how this issue can be managed. Here are some of the common conditions that may cause back pain:
Show Less
Herniated disks
Low back pain is often the first symptom of a herniated disk.
Disks are filled with a jelly-like substance to provide cushioning between your vertebrae and help keep them in place. A disk that ruptures is called a herniated disk; when this occurs in the lower area of the spine, the disk can… Show More
Low back pain is often the first symptom of a herniated disk.
Disks are filled with a jelly-like substance to provide cushioning between your vertebrae and help keep them in place. A disk that ruptures is called a herniated disk; when this occurs in the lower area of the spine, the disk can leak and press against nerves, contributing to back pain.
Activities that may strain your spine—such as lifting heavy objects, repetitive bending and twisting or sitting for long periods of time—and other factors, including smoking, age and obesity, can contribute to herniated disks.
If you’re experiencing pain in your back, hip, buttocks, legs or feet—particularly with feelings of numbness—see your healthcare provider for a physical exam and possibly imaging tests. Over-the-counter pain medication can usually help alleviate pain associated with herniated disks. In most cases, the discomfort will improve within four weeks. Depending on the severity of the condition, prescription pain medications, physical therapy, steroid injections or surgery may be needed.
Adopting some healthy lifestyle habits could help reduce your risk for a herniated disk. Being overweight or obese, for example, puts additional stress on the disks in your lower back. Losing extra pounds and maintaining a healthy weight can help ease this strain. If you’re overweight, work with your healthcare provider to develop a weight-loss plan that’s right for you.
Other ways to help prevent herniated disks:
- Stand up straight and use good posture
- Bend both your knees and hips when lifting something up off the floor
- When carrying something heavy, hold it close to your body
- Exercise regularly

Degenerative Disk Disease
Degenerative disk disease is a condition that involves deteriorating disks between the vertebrae. Some degeneration is natural as you age—disks become dry and lose their ability to absorb shocks. Traumatic injuries and the wear and tear caused by high-impact sports can also lead to disk tearing,… Show More
Degenerative disk disease is a condition that involves deteriorating disks between the vertebrae. Some degeneration is natural as you age—disks become dry and lose their ability to absorb shocks. Traumatic injuries and the wear and tear caused by high-impact sports can also lead to disk tearing, inflammation and soreness.
Disks that become injured have difficulty repairing themselves because the blood supply is limited, leading to deterioration. This condition can cause pain in the back, buttocks and thigh areas. Here’s what to watch out for:
- Pain that can be nagging, severe or disabling
- Numbness, pain, tingling or weakness in the back, buttocks, thigh or leg areas
- Pain that is exacerbated by sitting, bending or lifting
- Pain that improves with walking, moving around or changing positions when lying down
- Pain that comes in waves and can last for a couple of days to a few months
A physical exam, medical history and MRI can usually help your doctor determine whether you have the signs of degenerative disk disease. Usually, strengthening the muscles around the spinal area with exercise can reduce pain. Other treatments may include physical therapy, heat and cold therapy, medication (including anti-inflammatories) and various types of surgery.
Show Less
Arthritis
Arthritis (inflammation of joints) can give you creaky knees and sore hands, but it could also affect the spine—particularly the lower back. There are many types of arthritis, but a few are most likely to attack your back.
Osteoarthritis (OA) is the most common culprit and it usually happens later… Show More
Arthritis (inflammation of joints) can give you creaky knees and sore hands, but it could also affect the spine—particularly the lower back. There are many types of arthritis, but a few are most likely to attack your back.
Osteoarthritis (OA) is the most common culprit and it usually happens later in life—after age 40. It often accompanies degenerative disc disease and involves the breakdown of the joints where the vertebra connect with each other. Symptoms include lower back pain that can spread down your legs, or neck pain that radiates to the shoulder. The condition tends to be most painful in the morning and during activities, especially those that involve twisting or bending. It’s also relieved by rest.
Axial spondyloarthritis is an inflammatory arthritis that usually affects younger adults and is associated with other immune-related conditions, such as psoriasis and inflammatory bowel disease. This type almost always causes low back pain and stiffness that is worse at night and after rest, and improves with exercise. Over time, the vertebra can actually fuse together.
Less often, several forms of arthritis, such as rheumatoid arthritis, gout and psoriatic arthritis, as well as some arthritis-related conditions, including polymyalgia rheumatica, fibromyalgia and Paget’s disease, can trigger pain, stiffness and swelling in the back.
See your doctor if your pain associated with arthritis doesn’t get better with time. If your symptoms don’t improve with conservative treatment, your healthcare provider may suggest that you have a physical exam, blood test or imaging tests. If the test results confirm a diagnosis of arthritis, your doctor will advise you about your treatment options, which may include joint surgery, such as joint replacement, and lifestyle changes, such as regular exercise and eating a healthy, well-balanced diet.
Show Less
Back injuries
Any trauma to the back can lead to aches and soreness, especially, when it comes to short-term pain. Besides herniated discs, these injuries are among the most common causes of back pain:
- Sprains: Traumatic injuries, twisting, improper lifting or accidents can cause back ligaments to tear, … Show More
Any trauma to the back can lead to aches and soreness, especially, when it comes to short-term pain. Besides herniated discs, these injuries are among the most common causes of back pain:
- Sprains: Traumatic injuries, twisting, improper lifting or accidents can cause back ligaments to tear, leading to pain in one spot or a more generalized area. Chronic strain can also result from repetitive motions or the overuse of muscles and tendons.
- Spasms: Back spasms—involuntary muscle contractions that feel similar to cramps—may occur if the back has been strained or overworked.
- Spinal fractures: Falls and trauma can result in a spinal fracture, as can osteoporosis, or gradual weakening of the bone. Anything that puts excessive force or pressure on the spine can also lead to crushed vertebrae and compression fractures.

Osteoporosis
Osteoporosis involves bones that become weakened over time, making them more vulnerable to breaks. This condition, which affects millions of U.S. adults, can also lead to back pain. Your risk for osteoporosis increases with age. Women are also more likely to develop the condition than men. Other… Show More
Osteoporosis involves bones that become weakened over time, making them more vulnerable to breaks. This condition, which affects millions of U.S. adults, can also lead to back pain. Your risk for osteoporosis increases with age. Women are also more likely to develop the condition than men. Other risk factors include having a family history of the disease, being white or of Asian descent, having a thin frame or low bone density and taking certain medications.
Some people with osteoporosis don’t have any symptoms and may not realize they have the condition until they break a bone. Your healthcare provider can recommend a bone mineral density test to confirm whether or not you have osteoporosis.
You can also take steps to strengthen your bones, including adopting a diet rich in calcium, vitamin D and protein, getting regular exercise and not smoking. It’s equally important to take precautions in your everyday life to prevent falls. Wearing appropriate shoes, removing clutter from floors and walkways and being careful when walking in the rain or snow can all help. Be sure to check with your healthcare provider before taking calcium and vitamin D supplements.
Show Less
Endometriosis
You may be surprised to learn that endometriosis—a reproductive health condition that affects more than 11 percent of reproductive-age women in America—can be responsible for some back pain, too. When you have endometriosis, uterine lining tissue grows outside of the uterus, such as on the… Show More
You may be surprised to learn that endometriosis—a reproductive health condition that affects more than 11 percent of reproductive-age women in America—can be responsible for some back pain, too. When you have endometriosis, uterine lining tissue grows outside of the uterus, such as on the ovaries, fallopian tubes and tissues that keep the uterus in place.
Pain, particularly severe menstrual cramping, is the main sign of endometriosis. But the condition can also cause pain in the lower back, pelvis and intestine, as well as painful bowel movements and sex. Irregular menstrual bleeding or spotting and infertility are also associated with endometriosis.
If you suspect that you may have endometriosis or you’re experiencing any of these symptoms, see your healthcare provider. Your doctor may recommend that you undergo a pelvic exam and imaging tests, such as an ultrasound or magnetic resonance imaging (MRI) scan, to check for cysts and patches of tissue caused by endometriosis. Keep in mind, laparoscopy—a surgery used to examine your pelvic area and look for endometriosis tissue—is the only way to confirm that you have endometriosis with complete certainty.
There is currently no cure for endometriosis but medications, such as hormonal birth control and intrauterine devices, can help minimize bleeding as well as back and pelvic pain.
Show Less
Kidney stones and kidney infections
Kidney issues, such as kidney stones and infections, can trigger back pain. Kidney stones are hard kidney formations that are classified as either calcium, uric acid, struvite or cystine stones. Calcium stones are most common, and occur when calcium buildup isn’t naturally flushed out through your… Show More
Kidney issues, such as kidney stones and infections, can trigger back pain. Kidney stones are hard kidney formations that are classified as either calcium, uric acid, struvite or cystine stones. Calcium stones are most common, and occur when calcium buildup isn’t naturally flushed out through your urine.
Kidney stones can be as small as a grain of sand or as large as pearl. While most kidney stones pass through the body on their own, some are too large to pass and may get stuck in the urinary tract and need to be removed with help from a doctor.
Larger kidney stones may cause side or back pain. The pain can be mild or severe and may come and go. Other signs include vomiting, bloody urine, fever, smelly urine or burning during urination. See a urologist if you have these symptoms. Your healthcare provider may recommend that you undergo blood or urine tests, an x-ray of your abdomen, a computed tomography (CT) scan, or a combination of these tests.
Treatment for kidney stones depends on the severity of your symptoms and their size. For larger stones, your doctor may need to break them up or remove them using a procedure, such as shock wave lithotripsy.
A kidney infection, also known as pyelonephritis, is a urinary tract infection that occurs in the kidneys and can lead to back pain, too. Bacteria that’s supposed to live in the gut can make its way to the kidneys and cause the infection.
Pain associated with infections is usually in the flank, or the side of the lower back where the kidney is located. Fever or nausea are other symptoms of a kidney infection. A simple physical exam and urine test can confirm the diagnosis, and treatment will depend on the severity of your symptoms. In many cases, antibiotics are used to clear the infection.
Show Less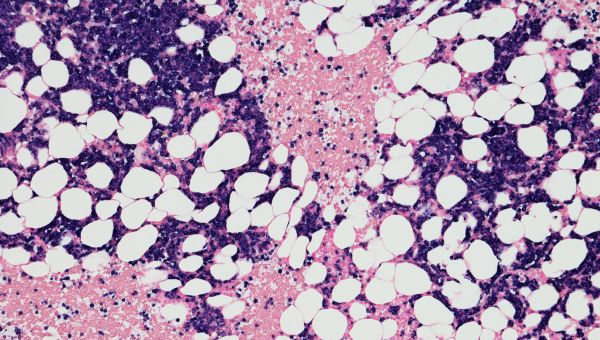
Tumors
Certain cancers, including those of the GI tract, pelvic organs and chest cavity, can cause back pain in a variety of ways. They may put direct pressure on the spine, through enlarged lymph nodes or metastases or place pressure on nerves. Blood-related cancers, such as multiple myeloma and leukemia… Show More
Certain cancers, including those of the GI tract, pelvic organs and chest cavity, can cause back pain in a variety of ways. They may put direct pressure on the spine, through enlarged lymph nodes or metastases or place pressure on nerves. Blood-related cancers, such as multiple myeloma and leukemia can also cause back pain.
Common signs of advanced multiple myeloma, in particular, include bone pain in the back, hips or chest, bone weakness or bone fractures. If the cancer causes the bones to become weak, they may collapse and put pressure on the spinal nerves, compressing the spinal cord. This can result in extreme back pain or leg numbness.
Depending on the stage of cancer, treatment options include surgery, chemotherapy, radiation or stem cell transplants.
Show LessMore On


video

article

slideshow


video


video
