What a neurosurgeon wants you to know about back surgery
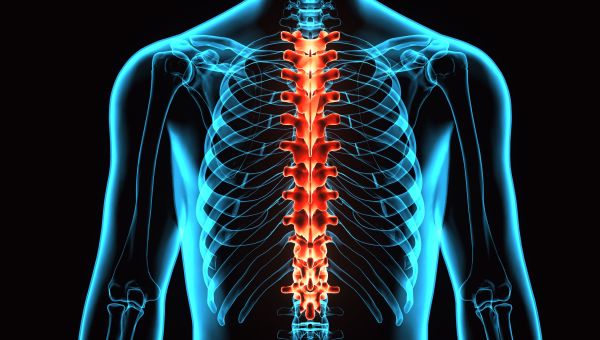
Find out who really needs it, how to best prepare and what you can do to speed up recovery.

The prospect of having back surgery can be nerve-wracking, but knowing what to expect, from your first doctor's visit through the removal of your final stitch, may help ease that worry.
Knowing your procedure may be performed using minimally invasive techniques, something surgeons aim to do, might also be reassuring. This kind of surgery causes less nearby tissue damage… Show More
The prospect of having back surgery can be nerve-wracking, but knowing what to expect, from your first doctor's visit through the removal of your final stitch, may help ease that worry.
Knowing your procedure may be performed using minimally invasive techniques, something surgeons aim to do, might also be reassuring. This kind of surgery causes less nearby tissue damage than open surgery, and often results in a shorter recovery, a lower risk of complications and a less painful recuperation.
We spoke with Sabino D'Agostino, DO, a neurosurgeon with Trident Medical Center in Charleston, South Carolina, to get the details on a variety of back surgeries, as well as tips for preparation and recovery.
Medically reviewed in April 2018.
Show Less
Who really needs spine surgery?
Back pain caused by overexertion, poor posture or wearing high heels often goes away by itself, but nonsurgical treatments like physical therapy, pain medication and steroid injections to help reduce inflammation may speed it along. In these cases, when pain is caused by muscle of ligament strain,… Show More
Back pain caused by overexertion, poor posture or wearing high heels often goes away by itself, but nonsurgical treatments like physical therapy, pain medication and steroid injections to help reduce inflammation may speed it along. In these cases, when pain is caused by muscle of ligament strain, surgery won't likely be necessary.
But, when back pain is caused by a deeper issue, like disk herniation or spinal nerve compression, surgery may be an option if your pain doesn't subside with the help of other treatments. It's most often performed to address spinal weakness or instability, nerve pressure, spinal deformity or bone or joint malformation caused by conditions like arthritis.
If you experience back pain and have been diagnosed with one of these conditions, speak with your doctor about whether surgery is right for you. Be sure to ask about:
- Preemptive nonsurgical treatments to try
- Your options for the procedure
- Pain and pain management
- Projected recovery time
- Potential risks
Taking notes is always a good option. You may also want to bring a friend or family member to the visit, who might ease your apprehension, help you decipher and remember information and make you feel more confident about asking questions.
Show Less
Traditional surgery vs. minimally invasive spine surgery
You and your provider will make a number of decisions about your procedure, one of which is choosing between an open surgery and a minimally invasive one.
Traditional open surgeries involve incisions about 5 or 6 inches long, which may cause nearby muscle and tissue damage and require long recovery… Show More
You and your provider will make a number of decisions about your procedure, one of which is choosing between an open surgery and a minimally invasive one.
Traditional open surgeries involve incisions about 5 or 6 inches long, which may cause nearby muscle and tissue damage and require long recovery periods. Minimally invasive spine surgery, on the other hand, uses smaller incisions and specialized instruments that generally cause less damage. Not all spinal surgeries can be performed using minimally invasive techniques, but many, like a diskectomy and laminectomy, can be.
Other potential benefits of less invasive procedures include:
- Better cosmetic results
- Less risk of blood loss
- Reduced risk of infection
- Lower likelihood of dependence on pain medication
- Shorter hospital stay
- Less trauma to organs
Common types of spine surgery
The type of procedure you have will ultimately depend on your specific back issue. These common spine surgeries, which each address different problems, may be performed using either minimally invasive or open techniques.
Laminectomy: Lamina is the bony part of the vertebrae protecting the spinal… Show More
The type of procedure you have will ultimately depend on your specific back issue. These common spine surgeries, which each address different problems, may be performed using either minimally invasive or open techniques.
Laminectomy: Lamina is the bony part of the vertebrae protecting the spinal cord. Pressure on the spinal cord and surrounding nerves, common among people with arthritis of the spine, can be relieved by a laminectomy. During this procedure, a portion of the arthritis or otherwise deformed lamina is removed to relieve this pressure.
Foraminotomy: The space where a nerve exits the spinal column is called the foramen. A condition called spinal stenosis causes the foramen to narrow, pressing on the nerve and causing pain. During a foraminotomy, a surgeon will widen the foramen. Bone fragments and other affected portions of the spine may also be removed.
Diskectomy: Spinal disks are the "cushions" that separate and support the vertebrae. When a disk herniates, or moves out of place, it can compress the spinal cord or surrounding nerves. During a diskectomy, a spinal disk or portion of a disk is removed to relieve pressure and pain. The type of diskectomy you have will vary based on the degree and location of herniation.
Disk replacement: Spinal disks also prevent vertebrae from rubbing together. Sometimes they deteriorate, and the friction between the bones can cause back pain. During a disk replacement, the affected disk or disks will be removed—through an incision in the neck—and replaced with artificial disks. This procedure isn't right for everyone and is best performed on people who don't have:
- Spinal deformities, like scoliosis
- Prior spine surgeries
- Bone or joint disease
Spinal fusion: Done for a variety of reasons including broken vertebrae, weakness or instability, spinal deformities or disk herniation, spinal fusion surgery joins two or more vertebrae together, eliminating the movement between them. "We also do this surgery for people who have degenerative disk disease, where the disk itself is worn out," Dr. D'Agostino says. A decompression surgery, like a laminectomy or foraminotomy, will almost always accompany a spinal fusion.
Show Less
Preparing for your surgery
Much like studying for a big exam, you can take steps to prepare your body for spine surgery. Prior to the operation, you will likely be evaluated by your primary care physician and any doctor you see on a regular basis, like a cardiologist. You may be asked to give blood and urine samples. To… Show More
Much like studying for a big exam, you can take steps to prepare your body for spine surgery. Prior to the operation, you will likely be evaluated by your primary care physician and any doctor you see on a regular basis, like a cardiologist. You may be asked to give blood and urine samples. To screen for issues that may complicate surgery, you may be asked to sit for an electrocardiogram (EKG) and/or an echocardiogram—a scan that can help detect heart disease.
Certain medications, like ibuprofen or aspirin, can affect surgery, so speak with your doctor about any prescription and over-the-counter drugs you take. Getting enough sleep, exercising regularly and eating a healthy, varied diet are all important prior to surgery.
There are some populations that would benefit from specific preparations, D'Agostino says. "If you're a diabetic, you really want to get your diabetes under control. If you're a smoker, you want to make your best effort to quit smoking," he says. "Quitting even a month before surgery would be helpful."
These interventions help speed healing and shorten hospital stays, says D'Agostino.
Show Less
There are still risks
Even the smallest procedures have some risks, including the possibility of infection, blood loss and adverse reactions to anesthesia. Surgery—even the minimally invasive kind—poses a risk of nerve damage, as well. "We do have to manipulate the nerves when we do these surgeries, and there is a risk… Show More
Even the smallest procedures have some risks, including the possibility of infection, blood loss and adverse reactions to anesthesia. Surgery—even the minimally invasive kind—poses a risk of nerve damage, as well. "We do have to manipulate the nerves when we do these surgeries, and there is a risk of permanent nerve damage," D'Agostino says.
Although spine surgery can be an effective way to treat back pain in certain situations, there is a possibility future procedures will be necessary. Degenerative disk disease is a continuous process, D'Agostino reminds us. "When we operate on the back or the spine, we operate on one part of it," he says. "Although we fix one part of the spine, there could be continued degeneration in other parts."
Show Less
What recovery might be like
Everybody is different, and every procedure comes with a different recovery period, but most people bounce back quickly after less invasive spine surgeries. The average hospital stay following these procedures is one to two days, shorter than the three- to five-day stay often recommended after an… Show More
Everybody is different, and every procedure comes with a different recovery period, but most people bounce back quickly after less invasive spine surgeries. The average hospital stay following these procedures is one to two days, shorter than the three- to five-day stay often recommended after an open spine surgery. Since small incisions disrupt less muscle and tissue, patients typically experience less postoperative pain, and minor discomfort can be managed with medication and the help of your doctor.
After procedures like microdiskectomies—a discectomy performed with more precision and smaller incisions—patients can expect a full recovery within just a few weeks. Recuperation after a more involved surgery, like spinal fusion, could take several months.
Your doctor may also recommend physical therapy to help strengthen the muscles around the spine. Regardless of the procedure, D'Agostino says patients should expect to attend follow-up appointments, during which your provider will assess your progress and let you know when it's safe to resume normal activities.
Show LessMore On


video

article

slideshow


video


video
