Updated on December 16, 2024.
In the early days of the COVID pandemic, one of the first signs of sickness identified worldwide was the partial or full loss of the ability to smell or taste. Years later, COVID’s connection to losing these olfactory senses has been clearly established. Here’s what you should know about this symptom, its potential causes, and what you can do about it.
Losing the ability to smell is common
In 2021, more than 60 percent of people diagnosed with COVID experienced a partial loss of smell (hyposmia or microsmia) or a total loss (anosmia), according to a 2023 study published in The Laryngoscope. For some people, it’s the only symptom they experience.
But COVID isn’t the only virus that causes people to lose their ability to taste or smell things. Nicholas Rowan, MD, assistant professor of otolaryngology, head and neck surgery at the Johns Hopkins University School of Medicine in Baltimore, explains that many viral infections—including the common cold—cause inflammation around nasal tissue and within the olfactory nerve. “That is something that we have been dealing with for decades and decades and decades,” Dr. Rowan says.
Other medical conditions, like chronic sinusitis, cancer, and trauma to the nose, can also cause a person to lose their sense of smell.
And if your sense of smell is weakened or absent, then your sense of taste may also be affected, since your ability to detect flavor is strongly tied to your ability to pick up a scent.
“If you have a stuffy nose, fevers, chills, and you generally feel poor, you lose your sense of smell,” Rowan explains. “You can't taste that chicken noodle soup that Mom is making you because you're ill and your nose is blocked up.”
So, when people describe losing their sense of taste, he adds, “what patients are describing might actually be a change in the perception of flavor.”
Why COVID may affect smell and taste
Researchers are still investigating other possible reasons why COVID may lead to lost sense of smell or taste.
A November 2023 review published in the Journal of Translational Medicine noted that early in the course of a COVID infection, simple swelling in the upper inside area of the nose can temporarily inhibit someone’s sense of smell, just like what often happens with the common cold. However, with COVID, when someone experiences the loss of their sense of smell, it usually continues even when the swelling in their nose goes down.
That means there is another primary cause or set of causes. Research has shown that the SARS-CoV-2 virus can infect olfactory neurons and the olfactory bulb, which is linked to the central nervous system, so the virus could spread to the brain, as well as travel through the central nervous system.
Besides infecting neurons, if the immune system goes into overdrive, it can result in intense inflammation, meaning the virus is able to not only infect but also damage olfactory neurons. This same inflammation can also cause changes to neurotransmitters and the body’s signaling systems to the brain.
The reason the symptom may hang around so long in people with long COVID could potentially be because some of the essential stem cells in the olfactory system might not be able to help support cells to regenerate or function normally because of a persistent infection from the virus. Basically, the virus may be able to hang out in the olfactory bulb long after the rest of the body has cleared the virus—where it just continuously launches attacks on the olfactory sensory neurons.
How long does the loss of smell and taste usually last?
As their health improves, most people with COVID do regain their ability to smell and taste. Somewhere between 63 and 78 percent of people whose dysfunctional sense of smell lingers after recovery will still get back some or all of their sensory ability within 30 days from the first sign of illness, according to a November 2023 review published in the Journal of Translational Medicine.
But as many as 25 percent of people don’t get these senses back after recovery from COVID for months or even years. And some people may have long-term loss. “It’s possible to lose your sense of smell permanently after being sick with a virus,” Rowan says. “Though relatively uncommon, it’s a top cause of anosmia among the general population.”
Are any treatments available?
How can you tell for sure if you lose your sense of smell? Rowan suggests taking a whiff of (nontoxic) household products to gauge yourself. (Think air freshener or soap.) Then, “ask somebody who's around you—a friend or a family member—if they can smell that same substance.”
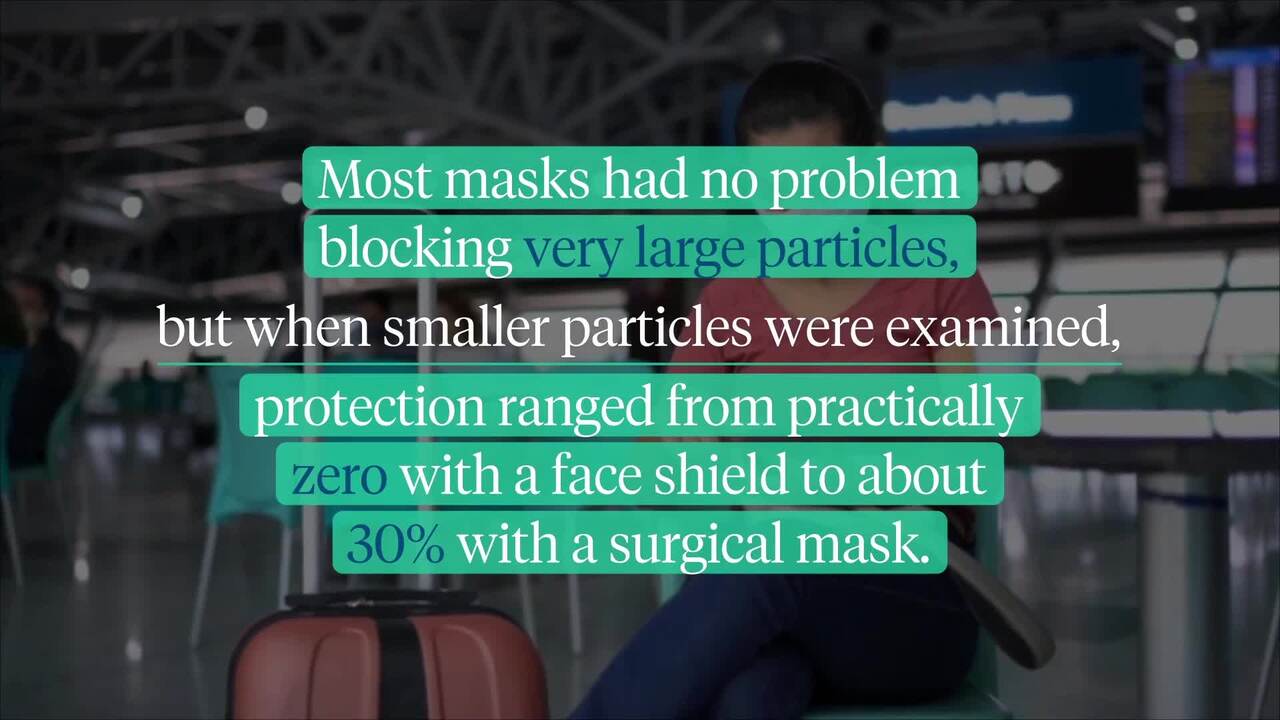
If your sense of smell or taste has disappeared, take a COVID test to confirm if you have the infection. If so, take steps to protect your loved ones by isolating, wearing a mask that fits snugly, making sure your home is well-ventilated, and practicing good handwashing hygiene.
If you have lost your sense of smell after a confirmed or suspected COVID infection, speak with your HCP about the treatments that may be appropriate for you.
Historically, for other viruses, says Rowan, “what we have found to be the most successful for treating patients with loss of sense of smell is something called smell training.” During smell training—also called olfactory training or olfactory rehab—a healthcare provider (HCP) typically asks you to sniff certain specific scents a few times daily for about 12 weeks to strengthen the function of your olfactory nerves.
“Just like if you had a knee surgery and needed to undergo physical rehabilitation, it's not like you lost your leg,” says Rowan. “You can still use it, but it will take some time to recover.”
Smell training has proven itself to also be helpful with COVID. People who had lost their sense of smell were, on average, able to more than double their olfactory scores through this training, according to a July 2023 systematic review and meta-analysis published in the American Journal of Rhinology and Allergy. Those who took the training within the first 30 days of losing their sense of smell had much more improvement than those who had chronic anosmia, but both groups significantly improved.
There are other possible options, too. Full of antioxidants, omega-3 fatty acids may help peoples’ senses of smell improve somewhat, and evidence suggests that a drug dosage of fatty acids could be more helpful than smell training alone. Some research has also shown that zinc may shorten your recovery time, and intranasal insulin films might also be of use.
For other respiratory illnesses besides COVID, the most commonly prescribed treatment for the loss of the sense of smell has been corticosteroids, both topical and oral. They can help in between a quarter and a half of all non-COVID-related cases. Unfortunately, we still don’t know for sure whether corticosteroids will effectively help a person who had COVID, but some research has suggested that they may help relieve these sensory issues
Ultimately, says Rowan, loss of smell and taste is something to be taken very seriously. And if that loss persists even after you recover from COVID, treatment is available. “If you lose it,” he says, “it doesn't necessarily mean that it's gone forever.”