Updated on April 8, 2025.
If you’ve got a fever and you’re coughing, congested, or battling a sore throat, chances are you’re also missing work, losing sleep—and running out of patience. It’s natural to want to feel better as quickly as possible. Many people with flu-like symptoms think antibiotics are a quick-fix for their misery. But in most cases, antibiotics are not the answer.
Antibiotics are powerful drugs, but they aren’t a cure-all. They specifically target bacteria, killing these microscopic organisms or preventing them from reproducing. But most chest colds and other illnesses are not caused by bacteria.
“The vast majority of respiratory illnesses are viral,” explains Robert Brown, MD, a primary care physician affiliated with Memorial Health in Savannah, Georgia. “Antibiotics will not do anything to a virus. They will not help at all.”
Bacteria vs. virus: What’s the difference?
You can’t escape bacteria. These one-celled microscopic organisms can be found just about everywhere in the environment—even in the human body. Different types of bacteria live on your skin, inside your mouth, and along your digestive tract.
Many of these microbes actually help you stay healthy. Only certain species of bacteria, including some that are normally found on the body, have the potential to make people sick, including Streptococcus, Staphylococcus, and E. coli. These and other types of bacteria are responsible for some common illnesses, like strep throat, bacterial pneumonia, and urinary tract infections (UTIs). The immune system can sometimes fight harmful bacteria on its own. More serious infections, however, are treated with antibiotics.
Antibiotics often work quickly. Even though these drugs may need to be taken for a week or more, people usually start feeling better and are no longer considered to be contagious after about 24 hours. Although antibiotics are highly effective against bacteria, they are useless against viruses—the germs responsible for the common cold, the flu, and other viral illnesses that cause similar symptoms.
Unlike bacteria, viruses are not living organisms. These tiny germs, which consist of genetic material wrapped in protein, need a living host to replicate. Antibiotics won’t clear a viral infection, help you feel better, or prevent you from spreading the illness to others.
In fact, there is no specific treatment for most viral illnesses. If taken right away, some anti-viral medications can reduce the severity and duration of the flu and COVID. But in most cases, people with a cold or other virus must rely on rest, fluids, and other supportive care until they recover on their own in about one to two weeks.
“The reality of the matter is we cannot make them well overnight,” he says. “It just takes time.”
The risks of antibiotic misuse
Since the symptoms of flu-like viruses are similar to the warning signs of a bacterial infection, it’s often tough to tell the difference. Feeling uncertain or frustrated, some people urge their healthcare provider (HCP) to prescribe them an antibiotic without knowing whether they really need it.
“For many years, unfortunately, my colleagues handed them out to make patients happier, maybe before we had as much data and before we were tracking these things as well as we do now,” Brown says. “We're certainly trying to reeducate everyone.”
Every year in the United States, at least 28 percent of antibiotics are still prescribed unnecessarily. This is not only unwarranted but also risky for two reasons:
The number of drug-resistant germs is increasing as the arsenal of effective antibiotics is dwindling. Before penicillin was discovered in 1928, people more often died of bacterial infections, such as pneumonia and tuberculosis, than from heart disease, cancer, and other non-contagious diseases. In the following decades, as more life-saving antibiotics were developed, the average life expectancy of Americans jumped from about 50 years of age to nearly 80.
Every time antibiotics are used, however, bacteria have a chance to adapt and become resistant to them. Overusing or misusing antibiotics (not taking them as prescribed, skipping doses, or not completing the entire course of treatment) allows more bacteria to develop resistance, making them stronger and more difficult to kill.
“The more you use an antibiotic, the less effective it may become in the future,” Brown explains. “That certainly holds true for individuals, but also for the community.”
With few new antibiotics under development, scientists are concerned that the rise of antibiotic-resistant bacteria will undo progress that has been made against bacterial infections over the past 70 years. Eventually, the increased risk for tough-to-treat infections may complicate common injuries and routine surgeries, like joint replacements.
A September 2024 study published in The Lancet cautions that antibiotic-resistant infections could result in more than 39 million deaths around the world by 2050. It’s the first analysis of the global health effects of antimicrobial resistance (AMR)—when germs like viruses and bacteria become resistant to the drugs that treat them.
In the United States, more than 2.8 million people develop infections that are caused by drug-resistant bacteria each year. These so-called superbugs claim at least 35,000 lives annually, the U.S. Centers for Disease Control and Prevention reports. They could drain $100 trillion from the world economy by 2050, according to one British report.
Like all medications, antibiotics may cause allergic reactions or other unwanted side effects. Taking these drugs unnecessarily exposes you to these risks without offering a potential benefit. Side effects from antibiotics may include:
- Rash
- Dizziness
- Nausea
- Diarrhea
- Secondary yeast or bacterial infections
- Irregular heartbeat
- Tendonitis, or increased risk for tendon injuries
What to do when antibiotics aren't the answer
If you’re suffering from a range of symptoms, including a runny nose, cough, low-grade fever, sore throat, and other flu-like symptoms, you may have a virus. If so, antibiotics won’t help but there are some things you can do to ease your discomfort, including:
- Rest.
- Drink plenty of fluids.
- Gargle with saltwater for temporary relief of a sore throat.
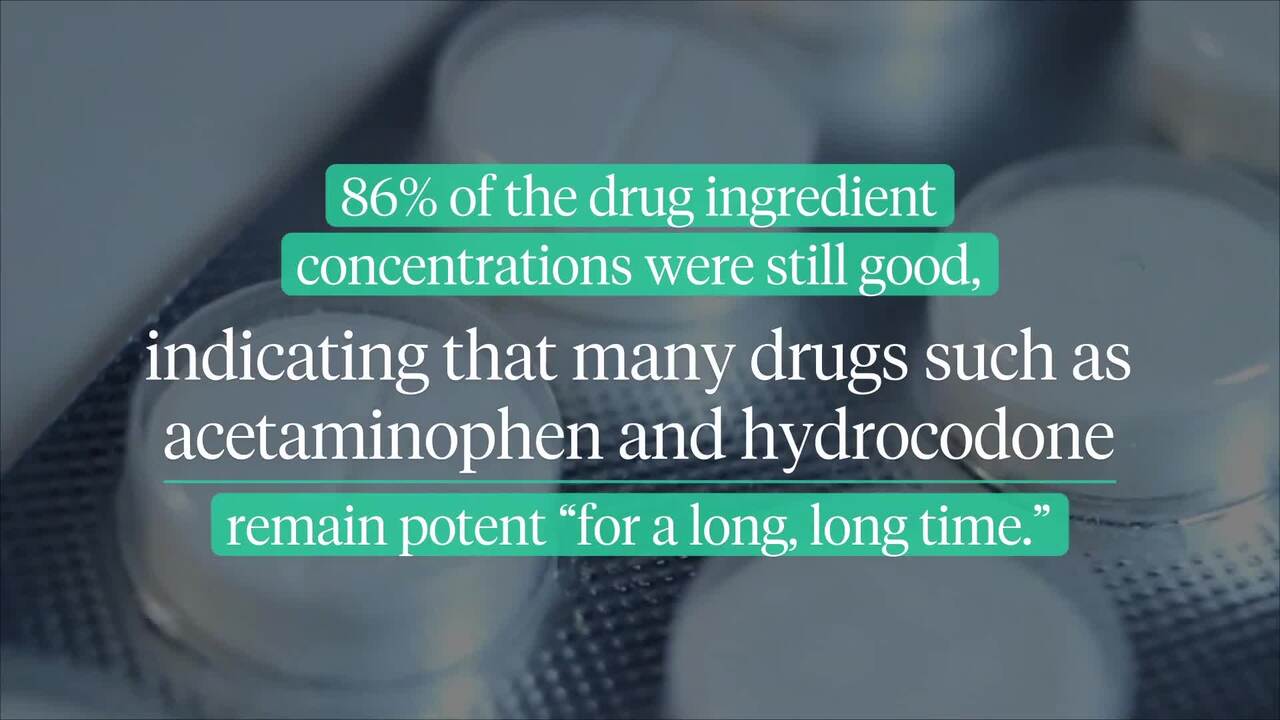
- Ask your HCP about over-the-counter pain and fever reducers, such as acetaminophen or ibuprofen.
- Use a cool mist vaporizer or humidifier to reduce congestion.
You can also try over-the-counter cough remedies or saline nasal sprays to get temporary symptom relief. These should be taken only as directed. Some of these products contain more than one active ingredient. Read all labels to ensure you’re not taking too much of any one medication.
Viruses usually clear up in a week or two. If your symptoms persist for more than 10 days without improvement, you could have a bacterial infection or another health issue that needs treatment. You should see your HCP.
Some other warning signs and symptoms that should be evaluated by an HCP:
- You have a persistent high fever and chills.
- Your fever or other symptoms gradually worsen over time, or improve initially but then get worse.
- You feel short of breath.
- Your sore throat develops very suddenly and you have tiny red spots on the roof of your mouth.
Your HCP can perform a physical exam and tests to determine if you have a bacterial infection or another health issue that requires treatment. Sometimes a blood or urine test may also be needed to confirm or rule out a diagnosis.
“I would say a temperature above 100.5 [Fahrenheit] for more than 48 hours that’s just not getting better should certainly prompt somebody to get checked out,” advises Brown. “Let somebody look at you so that we can try and figure out if there's something else going on or something we need to treat.”
Seek immediate medical attention if you’re having trouble breathing, are in severe pain, or if you’re confused or disoriented. These may be symptoms of a life-threatening infection or other medical emergency.