11 things your gynecologist really wants you to know
You should come in even when you have your period and be prepared to ask any questions you may have about your health.
Updated on November 7, 2024

When you meet with your gynecologist, it should be a productive partnership. You want them to be approachable, attentive, and knowledgeable, and they want you to be proactive in your own self-care.
To get some insight into what gynecologists wish their patients knew about preventative care, we spoke to Elizabeth Newell, MD, an OBGYN in Spokane, Washington.

Ditch the douching
The vagina is a pretty self-sufficent part of your body. It naturally regulates healthy bacteria to help protect against infections and irritations. Douching, a practice that involves squirting a mixture of fluids like water and vinegar into the vagina, can actually encourage the growth of harmful… Show More
The vagina is a pretty self-sufficent part of your body. It naturally regulates healthy bacteria to help protect against infections and irritations. Douching, a practice that involves squirting a mixture of fluids like water and vinegar into the vagina, can actually encourage the growth of harmful bacteria. And even though health experts recommend that people skip douching, about 1 in 5 people with a vagina use douches.
The risks can be pretty serious. If you already have a vaginal infection, douching may push the bacteria into your uterus, fallopian tubes, or ovaries. Bacteria in these areas could lead to pelvic inflammatory disease, an infection of your reproductive organs.
If you’re pregnant or are planning to become pregnant, douching can increase the risk of preterm birth or ectopic pregnancy. (Ectopic pregnancy occurs when a fertilized egg grows somewhere outside of the uterus, most commonly in a fallopian tube). Douching may also increase your susceptibility to contracting sexually transmitted infections (STIs), including HIV. Excessive douching may also lead to vaginal irritation and dryness.
Dr. Newell notes that douching can also put you at risk for bacterial vaginosis and yeast infections. Your vagina naturally makes mucus to clean itself, so you typically don't need to do much more than take regular showers or baths with warm water.
Show Less
Keep up with annual appointments
Even if you’re not due for your next Pap smear or cervical cancer screening, you should still check in with your gynecologist for an annual checkup, says Newell.
These yearly appointments—which may or may not include a pelvic exam—are important because they give you and your gynecologist the… Show More
Even if you’re not due for your next Pap smear or cervical cancer screening, you should still check in with your gynecologist for an annual checkup, says Newell.
These yearly appointments—which may or may not include a pelvic exam—are important because they give you and your gynecologist the opportunity to discuss sexual activity, vaccinations, your menstrual cycle, and any pregnancy or birth control plans you may have. Your gynecologist may also suggest other potentially life-saving screenings, adds Newell. “We’re doing a lot more genetic screening for certain cancers like Lynch syndrome, uterine cancer, ovarian cancer, and breast cancer,” she says. Also on the agenda: any updates to your family history and conversations about how you can adopt healthy habits as you age, including getting regular exercise and eating a well-balanced diet.
While you’re there, ask about the best schedule for your cervical cancer screenings. Current guidelines say that women between the ages of 21 and 29 should have a Pap smear every three years. Women between the ages of 30 and 65 should have a Pap smear and an HPV test together every five years, a Pap smear alone every three years, or HPV testing alone every five years. After the age of 65, women can stop screening depending on whether they have had abnormal results from past Pap smears. Of course, if you experience symptoms such as heavier-than-normal menstrual bleeding, pain, dizziness, or unexplained discharge, check in with your gynecologist right away.
Show Less
Don’t avoid the doc because you worry they’re judging your body
Newell points out that healthcare providers (HCPs) see many different types of bodies all day long, and they give little thought to whether their patients have shaved their legs, waxed their bikini lines, or have tattoos. So if you’re avoiding an appointment because you’re worried what your HCP… Show More
Newell points out that healthcare providers (HCPs) see many different types of bodies all day long, and they give little thought to whether their patients have shaved their legs, waxed their bikini lines, or have tattoos. So if you’re avoiding an appointment because you’re worried what your HCP will think, rest assured that their main concern is your health. (However, as a tip, Newell does recommend trimming or waxing rather than shaving the pubic area, since shaving sometimes raises the risk for folliculitis and blisters.)
Show Less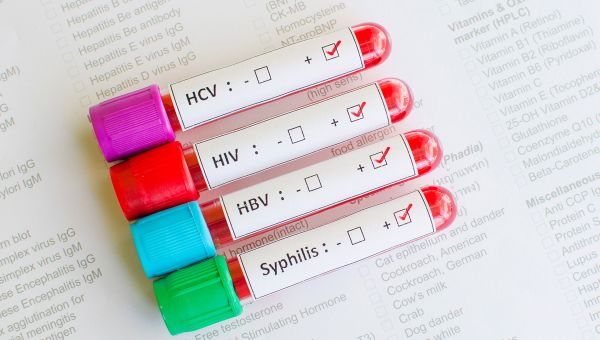
Get tested—even if you don’t have symptoms
Most sexually transmitted infections (STIs)—including chlamydia, human papillomavirus (HPV), and herpes—have mild symptoms such as abnormal vaginal discharge or pain when urinating. And many times, they can have no symptoms at all. But left undetected and untreated, STIs can potentially lead to… Show More
Most sexually transmitted infections (STIs)—including chlamydia, human papillomavirus (HPV), and herpes—have mild symptoms such as abnormal vaginal discharge or pain when urinating. And many times, they can have no symptoms at all. But left undetected and untreated, STIs can potentially lead to infertility issues or even cervical cancer down the road. This is why it’s a good idea to talk with your HCP about getting tested when you’ve been with a new partner, says Newell. Testing may involve a pelvic exam, blood or urine test, or tissue sample.
Show Less
Go ahead and consult the internet—but follow up with a real doctor
Do you ever find yourself up at night, Googling symptoms like itching, frequent urination, or funky discharge? It’s completely understandable to want to get an idea of what’s causing your symptoms before you have the chance to visit an HCP. But your at-home research should always be followed up by… Show More
Do you ever find yourself up at night, Googling symptoms like itching, frequent urination, or funky discharge? It’s completely understandable to want to get an idea of what’s causing your symptoms before you have the chance to visit an HCP. But your at-home research should always be followed up by a visit to a real-life HCP. They can narrow down a diagnosis with an exam and testing.
Because even if you’re sure you have, say, a yeast infection, you could actually have another condition with similar symptoms. And if you take the wrong over-the-counter medication, it won’t work, says Newell. Urinary tract infections (UTIs), kidney stones, and ovarian cysts all have similar symptoms that can be misdiagnosed by Dr. Google.
So, next time you experience unusual symptoms, schedule an appointment with an HCP—and be prepared to provide a sample—so a professional can properly treat your issue.
Show Less
You can still see the doctor if you have your period
If a surprise visit from your period has you reaching for the phone to reschedule your gynecology appointment until after your period, that’s totally fine—but it’s not necessary. “We still want women to come in when they have their period,” Newell says. “We can still get a pretty good sample during… Show More
If a surprise visit from your period has you reaching for the phone to reschedule your gynecology appointment until after your period, that’s totally fine—but it’s not necessary. “We still want women to come in when they have their period,” Newell says. “We can still get a pretty good sample during the Pap smear.” She adds that HCPs are used to seeing people who are menstruating or having spotting. In fact, she says it’s rare that your HCP won’t be able to get a proper sample.
If you’d prefer to see your HCP when you’re between periods, consider tracking it and scheduling appointments 10 to 20 days after you expect your period to start.
Show Less
Your family medical history is an important clue to your health
One of the most helpful things you can do for your own health is to ask your parents about theirs. (And while you’re at it, ask about grandparents, aunts, and uncles, too.)
“New cancers in the family or someone in the family passing away from a heart attack are good things for us to know,” says… Show More
One of the most helpful things you can do for your own health is to ask your parents about theirs. (And while you’re at it, ask about grandparents, aunts, and uncles, too.)
“New cancers in the family or someone in the family passing away from a heart attack are good things for us to know,” says Newell. Your gynecologist will use your family health history to make recommendations about screening for things like heart disease, uterine cancer, colon cancer, and breast cancer.
You can make a project out of this by creating a health-focused family tree. Include the date of birth, date of death (if applicable), and any medical conditions or surgeries your family member has had. You can share this with parents and siblings, as well as grandparents, aunts and uncles, nieces and nephews, children and grandchildren. And if anything changes, keep your providers updated as you have more info.
Show Less
If your doctor is running late, there may be a good reason
It can be incredibly frustrating to have to wait for an appointment that's delayed through no fault of your own. But consider what may be causing the delay.
“Sometimes we have to give bad news to someone, spend time with someone who is critically ill, or who just had a miscarriage or found out they… Show More
It can be incredibly frustrating to have to wait for an appointment that's delayed through no fault of your own. But consider what may be causing the delay.
“Sometimes we have to give bad news to someone, spend time with someone who is critically ill, or who just had a miscarriage or found out they’re pregnant,” says Newell. “That extra 30 minutes of comfort really helps them.”
Show Less
You don’t have to put up with PMS symptoms
It’s typical to experience a few physical or mental changes leading up to your period. But, if month after month, you’re experiencing symptoms that interfere with your daily activities, you may be experiencing premenstrual syndrome (PMS). Some symptoms of PMS include, but are not limited to:
It’s typical to experience a few physical or mental changes leading up to your period. But, if month after month, you’re experiencing symptoms that interfere with your daily activities, you may be experiencing premenstrual syndrome (PMS). Some symptoms of PMS include, but are not limited to:
- Depression or anxiety
- Insomnia
- Food cravings
- Bloating and weight gain
- Headaches
- Fatigue
Mild and moderate cases of PMS can usually be addressed with lifestyle changes such as exercise, relaxation therapy, and diet tweaks. Severe PMS symptoms, however, may require medications such as antidepressants, nonsteroidal anti-inflammatory drugs (NSAIDs), or diuretics, otherwise known as “water pills.”
You should always talk to your HCP about any symptoms you have related to your period. They can assess those symptoms and suggest treatment options that may give you some relief. In some cases, certain symptoms like severe cramping (appearing in combination with spotting between periods, infertility, or stomach issues) could indicate more serious health conditions such as endometriosis, which would require additional testing or treatment.
Show Less
Be cautious with scented soaps and other products
If winding down at the end of a long day with a luxurious bath is one of your life’s great pleasures, be sure to choose products that will be gentle on all parts of your body, especially your vaginal area. Soaps, lotions, or bubble baths (and even tampons and pads) that are scented can up your risk… Show More
If winding down at the end of a long day with a luxurious bath is one of your life’s great pleasures, be sure to choose products that will be gentle on all parts of your body, especially your vaginal area. Soaps, lotions, or bubble baths (and even tampons and pads) that are scented can up your risk of yeast infections or bacterial vaginosis. When it comes to cleaning your vaginal area in the bath or shower, a little mild, unscented soap works just fine. If you have sensitive skin, skip the soap. Warm water is all you need.
Show Less
There’s no such thing as a weird question
Remember that your gynecologist has probably seen—and heard—pretty much everything. So if you’re nervous about discussing your reproductive and sexual organs, or your sexuality—or asking questions about birth control, fertility, STIs, painful sex, period cramps, anal intercourse, and other sexual… Show More
Remember that your gynecologist has probably seen—and heard—pretty much everything. So if you’re nervous about discussing your reproductive and sexual organs, or your sexuality—or asking questions about birth control, fertility, STIs, painful sex, period cramps, anal intercourse, and other sexual habits—you can rest assured that your HCP talks about these things all day long and is there to answer your questions.
You can also ask your gynecologist about a range of other health issues, including menopause, breast health, tobacco or alcohol use, and other conditions you may be wondering about. And if you’re worried you’ll draw a blank when you’re in the exam room, write yourself notes before your appointment.
“I think patients either forget to ask questions or they’re too embarrassed to ask them,” says Newell. “We want our offices to be safe spaces for people, places where they feel like they’re accepted." If your sexual preferences or habits change, your gynecologist understands that, too.
Show Less
ACOG. Why Annual Pape Smears Are History-- But Routine OB-Gyn Visits Are Not. Last reviewed September 2022.
More On


video

article

slideshow


video


video
