Opioid addiction and overdose rates have reached epidemic levels, yet doctors still prescribe the drugs. Why? They work well to control pain, and in many cases, are the best treatment option. But not everyone needs opioids, and with their potential for abuse, it might be a good idea to look to other methods of pain management first.
“My mantra with patients is always keep it simple,” says Daniel Kloster, MD, an anesthesiologist and pain specialist with Menorah Medical Center in Overland Park, Kansas. Before seeking out opioids, says Dr. Kloster, make sure you’ve exhausted other treatment pathways first: over-the-counter medicines (OTC), prescription drugs, cortisone shots and alternative therapies.
When opioids are the right choice
Opioids—also known as narcotics—should be prescribed in certain situations, such as pain due to metastatic cancer or after surgery, says Kloster. The Centers for Disease Control and Prevention believe opioids should not usually be used for chronic pain, and Kloster agrees.
“Narcotics are really meant for the short term,” he says. “Just because people say they’re in pain doesn’t mean they need narcotics. To justify narcotics for chronic pain, you need imaging studies like MRIs that show something is wrong. To have normal studies and be on chronic narcotics is a no-no.”
Medication options
Kloster recommends trying over-the-counter medications first. “Before you call me, try non-steroid anti-inflammatory drugs (NSAIDs) like aspirin or ibuprofen, or Tylenol,” he says. NSAIDs carry a slight risk of stomach ulcers. Tylenol does not, but it’s not an anti-inflammatory, so it doesn’t work as well, according to Kloster.
One November 2017 study in The Journal of the American Medical Association suggests that OTC meds are as effective as opioids for pain relief in some cases. The study looked at about 400 emergency room patients experiencing moderate-to-severe acute pain in an arm or leg. Patients were given either ibuprofen plus acetaminophen or acetaminophen plus one of three narcotics—oxycodone, hydrocodone or codeine. Researchers found that two hours after taking a combination of medications, all patients had about the same amount of pain reduction, regardless of whether or not they took an opioid.
A March 2018 opioid study in the same journal produced similarly encouraging results. For a year, researchers followed 234 patients with chronic back pain or osteoarthritis pain in their hips or knees. Half the group was given opioids like morphine and oxycodone for pain relief. The other half received common non-opioid pain medications starting with OTCs like acetaminophen and NSAIDs. After 12 months, pain relief was slightly better for those taking the non-opioid drugs, and pain-related function was about the same between the two groups.
If you’ve tried OTC meds and you’re still in pain, your next step is to see a primary care physician or a pain specialist. Your healthcare provider may prescribe neuropathic medications. There are two main categories of neuropathic medications: anti-seizure medications and antidepressants. These medicines build up in the spinal cord over time and slow down pain signals, according to Kloster.
“Normal pain is like water boiling on the stove,” says Kloster. “If you’re hurting all the time, you live at the boiling point. These medications help reset the thermostat.”
Other pathways to pain management
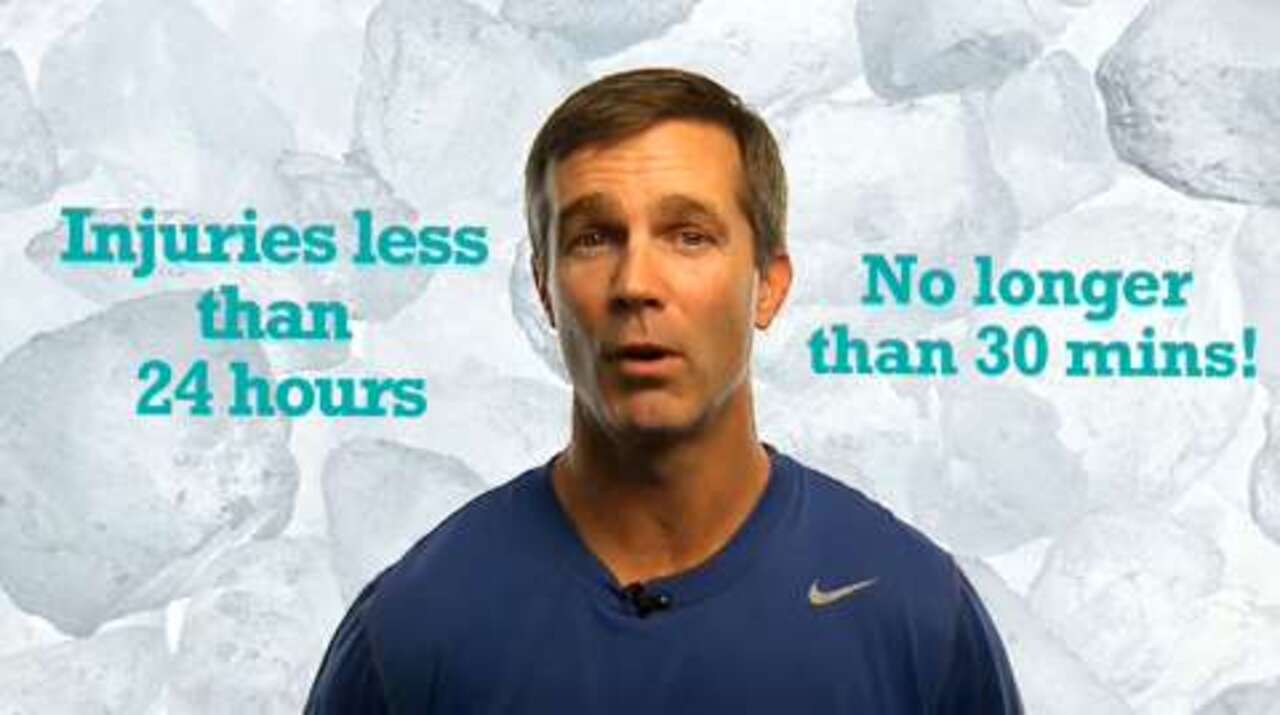
Another treatment option is corticosteroid injections. “Steroids are a powerful anti-inflammatory,” Kloster says. He describes the choice between injections and neuropathic medicines as a fork in the road. “The first thing you try is over-the-counter options, heat and ice,” he says. “That’s not working so you come to me, and we say we can try neuropathic medicines or try a shot. It’s personal preference.” Kloster notes that whichever fork you take, you can go back and try the other if your first choice doesn’t work.
Alternative therapies can also work, says Kloster. “Most doctors are trained in Western medicine: shots and pills. I’m trained that way,” he says. “That said, you can also do other things, like chiropractic and physical therapy. They’re non-medicinal options that can really have benefit.”
The best pain prescriptions
Now you know the options for when you have pain, but can’t or shouldn’t take opioids. But what is the best way to stop pain before it starts?
“Physical activity is the best thing for you,” says Kloster. “Every 10 pounds in front of you is 70 pounds on your back. Most of my patients have weight issues. I take care of plenty of marathoners as well, but being out of shape and overweight is a big risk factor.”
There’s one more thing you can do: Stop smoking. “The worst thing you can do is smoke,” Kloster says. “Smoking accelerates the arthritic process. It’s very bad for your bones.”