Pregnancy
- How can I achieve a healthy pregnancy?
- What are the symptoms of pregnancy?
- How do you know if you're pregnant?
- When should you see a healthcare provider?
- What are the stages of pregnancy?
- What are the three trimesters of pregnancy?
- Preparing for childbirth
- What are the most common pregnancy complications?
- What if I have trouble getting pregnant?
- Learn more about pregnancy
- Featured pregnancy articles
Introduction
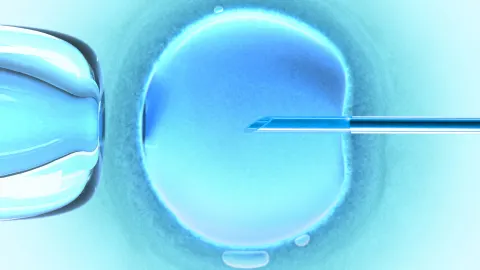
Pregnancy is the period of time when a fetus develops inside a person’s uterus (womb). It typically lasts around 40 weeks, or a little over 9 months. The first step in becoming pregnant is conception. This occurs when an egg in a woman or person assigned female at birth (AFAB) is fertilized by sperm from a man or person assigned male at birth (AMAB). Conception (or conceiving) takes place in the hours or days following unprotected sexual intercourse. Conception may also occur when sperm fertilizes an egg during the process of in vitro fertilization (IVF).
Pregnancy can be an overwhelming time. You may feel excited, stressed, or a mixture of several emotions. Add to that all the advice you may be receiving from friends, family members, and loved ones about what to do—and what not to do while pregnant—and things can quickly become confusing.
Learning the basics of pregnancy can clear up some of the confusion and help you make confident, educated choices. Read on to discover more about pregnancy, including its early signs and symptoms, the facts about prenatal care, and what you can expect during each stage of pregnancy.
How can I achieve a healthy pregnancy?
Following certain steps can improve your chances of having a healthy pregnancy. If you’re planning on becoming pregnant or already are, the Centers for Disease Control and Prevention (CDC) advises you to take these actions:
Visit a healthcare provider (HCP). Preconception (or pre-pregnancy) health care can increase your chances of having a healthy pregnancy. This care generally involves:
- Reviewing past or current medical conditions (including any issues with a previous pregnancy) that could interfere with fertility or pregnancy
- Ensuring any existing medical conditions (such as type 1 or type 2 diabetes, asthma, and high blood pressure) are under control
- Getting recommended vaccines, such as an annual flu shot and the Tdap (adult tetanus, diphtheria, and pertussis) vaccine
- Stopping birth control pills (oral contraceptives) or removing an intrauterine device (IUD, another method of birth control that sits in the uterus)
- Discussing what medications and supplements to take or avoid during pregnancy
- Learning ways to help prevent fetal conditions and complications
If you’re already pregnant, your HCP can provide you with additional health guidance or direct you to a specialist for prenatal health care. (“Pre” means before and “natal” refers to birth.)
Get your daily dose of folic acid. Folic acid is an essential B vitamin and the synthetic form of the vitamin folate. Having enough of it in your body at least three months before conception and throughout your pregnancy promotes healthy brain and spine development in a growing fetus. This can reduce the chances of fetal conditions like spina bifida (an underdeveloped spine) and anencephaly (an underdeveloped brain and skull).
The U.S. Department of Health and Human Services (HHS) Office on Women’s Health advises that women and people AFAB consume 400 to 800 micrograms (mcg) of folic acid every day before getting pregnant. This can come through supplements, fortified foods, or a combination of both. Maintaining a nutrient-rich diet with plenty of folate is also encouraged. Folate (the naturally occurring form of the vitamin) is found in foods like leafy green vegetables, beans, fresh fruits, whole grains, peanuts, and sunflower seeds.
Don’t drink alcohol, smoke, or use drugs. These behaviors are particularly dangerous for pregnant people, especially in the first few weeks and months of pregnancy. If you’re planning on becoming pregnant, it’s important to quit smoking, drinking alcohol, or using drugs. If you need assistance with quitting, reach out to an HCP. You can also contact an organization such as Alcoholics Anonymous or find a substance abuse treatment facility in your area.
Achieve and maintain a healthy body weight. People who are underweight, overweight, or obese have a higher risk of experiencing pregnancy complications. Before getting pregnant, try to reach a healthy body weight. Your HCP can identify a weight goal and recommend an eating plan or exercise routine that’s appropriate for your needs.
Avoid environmental contaminants and toxic substances. Certain chemicals can disrupt reproductive health (for both women and men and people AFAB and AMAB). They can contribute to infertility, increase the risk of health issues, or lead to loss of pregnancy such as miscarriage or stillbirth. If you’re planning on having a baby, try as much as possible to limit or avoid exposure to substances including:
- Bug spray (including mosquito repellant)
- Cleaning products that contain glycol ethers (often found in oven cleaners), many spray and aerosol cleaners, and products with “fragrance,” which may include potentially harmful phthalates
- Secondhand and thirdhand smoke
- Chemical fertilizer for plants
- Rodent and cat feces (poop)
- Pesticides and herbicides (chemicals designed to kill insects and certain plants)
- Mercury (which is found in many types of fish, including swordfish and king mackerel, as well as amalgam tooth fillings, mercury thermometers, and certain industrial materials)
- Flame retardants (chemicals applied to certain types of fabrics, clothing, and furniture to help prevent fires)
- Arsenic-treated wood
- Certain types of paint and paint fumes
- Lead
Visit your HCP to discuss what toxic substances and contaminants you may be exposed to at work, home, or in your environment. They can help you identify potential risks and suggest ways to lower your exposure to them.
Review your family history. If a sibling or a parent experienced difficulty conceiving, there’s a chance you may have trouble, as well. Additionally, some medical conditions are genetic, meaning they can run in families. Discussing your family’s health history can help your HCP identify possible health risks to you or your developing baby and suggest ways to minimize those risks. Your HCP can also refer you to a genetic counseling specialist for further information.
Prioritize your mental health. It’s important for everyone—pregnant or not—to take care of their mental health. If you’re experiencing persistent feelings of sadness, hopelessness, indifference, anxiety, or fear that interfere with your daily routine, reach out to your HCP or a licensed mental health provider, such as a counselor or psychologist. It’s also crucial to stay connected with trusted friends and family members and avoid isolating yourself as you work to improve your mental health.
Nutrition and pregnancy
If you’re pregnant, your body needs extra helpings of key nutrients like protein and fiber, and vitamins and minerals like choline, iodine, iron, folic acid, and calcium. Along with guidance from your HCP, try following these nutrition tips:
Consider calories. Your individual needs may vary, but most pregnant people should consume more calories as their pregnancy progresses. The general recommendations are:
- No extra calories for the first 12 weeks
- Around 360 extra calories per day between weeks 13 and 26
- Around 450 extra calories per day after week 26
Gaining weight is a natural and expected part of pregnancy. How much weight you should gain will depend on your weight before pregnancy and other factors, such as any health conditions you may have. Your HCP can help you determine a healthy weight goal and how many extra calories you should try to consume.
Enjoy healthy foods. You may need to eat more calories during pregnancy. Just remember: Not all calories are created equal. Eating a varied, nutrient-rich diet can help ensure you get the nourishment and energy you need to have a healthy pregnancy.
When considering your pregnancy diet, it’s best to include as many of these foods as possible:
- Vegetables, such as spinach, sweet potatoes, broccoli, okra, and peppers
- Fresh fruits, such as berries, oranges, bananas, apples, and mangoes
- Lean proteins, such as chicken and other lean meats and eggs; cooked including fish like salmon, sardines, cod, tilapia, and catfish, and shellfish like crab, lobster, and shrimp); and plant-based proteins like tofu, lentils and beans (including chickpeas), and nuts
- Whole grains, such as whole-wheat breads and pastas, oatmeal, brown rice, bulgur, and millet
- Healthy fats, found in foods like olive oil, avocados, nuts, and cooked, low-mercury seafoods
- Low-fat and fat-free dairy products, such as milk, cheese, yogurt, and soy alternatives
Some healthy snack ideas include carrots and hummus, homemade trail mix, fruit and Greek yogurt, apples and cheese, and whole-grain crackers topped with peanut butter. If you’re feeling nauseous (which can happen when you are pregnant), try snacking on dry cereal, saltine crackers, or dry toast. Be sure to wash fruits and vegetables well before eating.
Take a daily prenatal supplement. Every pregnant person should take a prenatal supplement (also known as a prenatal vitamin). Speak with your HCP about what type of supplement is best for you. In general, you should prioritize getting enough iron, folic acid, iodine, and choline.
Avoid or limit certain foods and beverages. If you’re pregnant, be sure to avoid the following foods and beverages:
- Alcohol
- Raw or rare poultry, meats, or eggs
- Deli meat, hot dogs, and smoked seafoods (unless they’re heated to at least 165 degrees Fahrenheit)
- Seafoods that are high in mercury, including marlin, shark, king mackerel, Gulf of Mexico tilefish, bigeye tuna, swordfish, and orange roughy
- Seafood and meat salads like tuna salad and chicken salad
- Raw or rare fish and shellfish, including oysters and sushi
- Raw sprouts, including mung bean, clover, alfalfa, and radish sprouts
- Unpasteurized cheese, milk, or juice (look for “pasteurized” on the package before purchasing)
It’s also important to limit your consumption of caffeinated beverages like coffee and tea. Stick to fewer than 200 milligrams of caffeine per day. It’s also a good idea to reduce your intake of drinks with added sugars, such as sports drinks, fruit drinks, soda, and sweetened water.
What are the symptoms of pregnancy?
Pregnancy symptoms can vary from person to person. The main sign of pregnancy is a missed menstrual period. (But there are several other factors that can cause you to skip periods.)
Symptoms of pregnancy can start as early as one week after conception. In addition to a missed period, other early signs of pregnancy include:
- Fatigue
- Nausea (with or without vomiting) at any time of day or night
- More frequent urination
- Swollen, sore breasts
As you continue in the first three months of pregnancy (known as the first trimester), you may also experience:
- Darkened breast areolas (the area around the nipple)
- Mood swings
- Headaches
- Lower back pain
- Bloating
- Unusual food cravings or aversions to certain foods
- Light bleeding (spotting) that is not your menstrual period
How do you know if you're pregnant?
One way to know if you’re pregnant is to take a home pregnancy test, which you can buy without a prescription at most stores that sell personal care products. You may also be able to request a pregnancy test at your HCP’s office or community health center.
Pregnancy tests work by detecting human chorionic gonadotropin (HCG) in urine. HCG is a hormone that’s produced by your body when you’re pregnant.
It can take several days for HCG to build up in your body after conception. Some pregnancy tests are able to detect HCG in urine as early as 10 days after conception. For the most accurate results, it’s best to wait until after your first missed period to take a pregnancy test. Most at-home pregnancy tests are around 99 percent accurate when used according to package directions.
Another option is to receive urine-based pregnancy testing at your HCP’s office. You may also ask to receive a blood test, which can detect even small amounts of HCG in blood as early as 7 days after conception.
An HCP may also perform ultrasound imaging to visualize an embryo or fetus and help determine how long you’ve been pregnant. An embryo is a dividing bundle of cells that will turn into a fetus around the eighth or ninth week of pregnancy. (More on these terms below.)
Ultrasound imaging may be able to detect an embryo as early as six weeks after conception. An ultrasound is a painless imaging test that uses sound waves to create an image of things inside the body.
When should you see a healthcare provider?
If you think you're pregnant or would like to begin trying to have a baby, speak with an HCP about what steps you can take to prepare for pregnancy. You should also promptly make an appointment with an HCP if a home pregnancy test indicates that you’re pregnant.
Health care for pregnant people is called prenatal care. Receiving regular prenatal care and attending all scheduled medical appointments can help lower the risk of health problems for you and for your developing baby.
According to the HHS Office on Women’s Health, babies of pregnant people who do not receive prenatal care are three times more likely to have low birth weight and five times more likely to die than babies who are born to people who received prenatal care.
Prenatal care allows your HCP to identify potential health concerns early and help prevent issues from occurring during pregnancy and childbirth. Generally, most pregnant people are advised to attend prenatal care visits on this timeline:
- Once a month between weeks 4 and 28
- Twice a month between weeks 28 and 36
- Once every week from week 36 through birth
Your first prenatal care visit may include a blood test, a test for sexually transmitted infections (STIs), a physical exam, and a pelvic exam, along with a discussion about your health habits, relationships, and goals for pregnancy and childbirth. Your due date (an estimation of when your baby will be born) will also be calculated.
As your pregnancy progresses, prenatal care visits may involve:
- Measuring your abdominal circumference
- Evaluating the heart rate and overall development of the fetus
- Checking your blood pressure, blood sugar, weight, and other important health measures
To ensure access to important prenatal care services, the Affordable Care Act (ACA) requires all health insurance providers to cover services for pregnant people. Available care options vary by state. Medicaid and the Children’s Health Insurance Program (CHIP) also provide free or low-cost coverage for prenatal care.
What healthcare providers offer prenatal care?
Multiple HCPs can provide prenatal care, including:
- Obstetricians (OBs): Obstetricians are medical doctors who specialize in female reproductive health, pregnancy, and childbirth (labor and delivery).
- Certified nurse-midwives (CNMs): Certified nurse-midwives are nurses who are certified in midwifery. This is a medical specialty that deals with reproductive health, pregnancy, and labor and delivery.
While CNMs can prescribe medications, they often care for pregnant people who wish to have what’s known as a natural childbirth. That typically means the pregnant person goes through labor and delivery at home or at a special birthing center (rather than a hospital) without the use of an epidural or other medications to reduce pain. Many CNMs work with obstetricians who can take over a person’s care in the event of a medical emergency.
- Family medicine physicians: Family medicine physicians are medical doctors who specialize in family medicine (routine health care for all people of all ages). Some (though not all) family practice physicians have additional training in prenatal care and childbirth. Others may offer prenatal care and partner with an OB or CNM for labor and delivery services.
Some pregnant people also choose to partner with a doula. This is a non-medical professional who is trained to provide physical and emotional support to people throughout their pregnancy and during childbirth. One 2023 study published in Cureus found that working with a doula was associated with shorter labor and better health outcomes for the baby and birthing parent.
Choosing a prenatal care provider is just one of many decisions you’ll face during your pregnancy. As you consider your options, keep in mind your health needs, what providers are in your area, and what sort of environment you’d prefer for delivering your baby (such as at home, a birthing center, or a hospital). The HCP you choose should be able to fully address any questions or concerns you may have and help you feel at ease.
What are the stages of pregnancy?
From a medical perspective, pregnancy can be divided into three stages:
- Germinal stage: This starts at conception and ends around the third week of pregnancy. During this stage, the fertilized egg (called a zygote) travels to the uterus and divides multiple times to become a blastocyst, which implants into the lining of the uterus.
- Embryonic stage: This starts around the third week of pregnancy and concludes toward the end of the eighth week. The blastocyst has developed into an embryo, which begins to form organs. A heartbeat appears around the fifth or sixth week.
- Fetal stage: This begins around the ninth week of pregnancy and continues until birth. Most of your baby’s development—from limbs to eyelashes and fingernails—will occur during this stage.
What are the three trimesters of pregnancy?
Pregnancy is also divided into three periods called trimesters. Each trimester of pregnancy brings unique changes and developments.
First trimester
The first trimester refers to the first three months of pregnancy, starting at conception and ending around week 12. During this stage:
- The placenta forms. This is a temporary organ that connects the parent to the fetus, providing it with essential nutrients during the pregnancy. The placenta will leave the body after the birth of the baby.
- The neural tube, which eventually becomes the brain and spinal cord, forms around week 5.
- Small buds of tissue that will eventually form arms and legs develop around week 6.
- Bones and genitals begin to form around week 7.
- Eyes are visible around week 8 and ears start to form.
- Feet, toes, hands, and fingers are fully developed around week 10.
- Urinary, digestive, and circulatory systems are functioning around week 12.
The fetus is around the size of a plum at the end of the first trimester. Reaching the end of the first trimester also means your chances of experiencing a miscarriage are significantly lower going forward. This is because most crucial fetal developments occur in the first 12 weeks of pregnancy.
As a pregnant person, you may experience one or more of these issues in the first trimester:
- Constipation
- Fatigue
- Swollen, tender breasts with changes to the color or shape of nipples or areolas
- Nausea and upset stomach
- Frequent urination
- Heartburn
- Weight loss or weight gain
- Headache
- Mood swings
Practicing healthy sleep habits, drinking enough water, and eating smaller meals throughout the day can help you cope with some of the issues that may come with early pregnancy. It’s also possible to go through the first trimester without experiencing any noticeable issues.
Second trimester
The second trimester runs from week 13 through week 28. The fetus continues to develop more noticeable features:
- Muscles and nerves start to work in unison around week 12. (For example, the fetus can make a fist.)
- Vocal cords develop around week 13.
- Fine hair begins to grow around week 14.
- Lungs start to form around week 15.
- Around week 16, the fetus’s ears are developed enough to hear you speak.
- External genitals and the fetus’s assigned sex are usually visible on an ultrasound between weeks 18 and 20.
- After week 23, it may be possible for a fetus to survive outside of the womb with intensive medical care.
- Footprints and fingerprints are present at 24 weeks.
- Eyelids are open, blinking, and have eyelashes around week 27.
The fetus may start to turn head-down in the uterus in preparation for birth around week 28. At this point, the fetus is about the size of an eggplant.
For many pregnant people, nausea fades and visible signs of pregnancy (namely a growing belly) begin to appear. You may feel your baby move and kick around week 20. As your body changes and your baby grows, you may experience:
- Back pain
- Body aches around your thighs, groin, and abdomen
- A line on your skin that runs from the belly button to the pubic area
- Discolored patches of skin, often on the cheeks, upper lip, nose, or forehead (this is sometimes called a “pregnancy mask”)
- Carpal tunnel syndrome (marked by tingling or numbness in the hands)
- Stretch marks (discolored, indented streaks) on your buttocks, thighs, abdomen, or breasts
- Itchiness that occurs on your palms, abdomen, or bottoms of your feet
- A swollen face, fingers, or ankles
Promptly call your HCP if you develop itchiness with nausea, vomiting, reduced appetite, fatigue, or jaundice (yellowing of the skin or whites of the eyes). This could indicate a serious liver condition. It’s also important to seek immediate medical care if you experience sudden or intense swelling or if you gain a significant amount of weight very quickly.
Third trimester
The third trimester starts at week 29 and ends with childbirth. As your due date approaches, keep in mind that these last few days and weeks of pregnancy are vital to fetal brain and lung development. During this stage:
- Kicking, punching, and movement may become more noticeable in your uterus.
- The brain continues to form and grow.
- Distinct patterns of sleep and activity may be noticeable around week 31.
- Bones become harder around week 33.
- Reserves of fetal body fat increase. (A fetus gains about a half a pound per week around week 38.)
Your baby is considered “full term” at week 39. Full-term babies are more developed, generally healthier, and have fewer health risks than babies born “preterm” (before 37 weeks). Babies born during weeks 37 and 38 are considered “early term.” Most HCPs encourage pregnant people to wait until week 39 to deliver if they can, unless delivering the baby early is medically necessary or labor naturally occurs pre- or early-term.
As you enter the final months of your pregnancy, you may experience additional issues and signs, including:
- Difficulty sleeping
- Shortness of breath
- Hemorrhoids
- An “outie” belly button (one that sticks outward)
- Heartburn
- A swollen face, fingers, or ankles
- Increasingly tender breasts that may leak colostrum (a watery type of breastmilk that’s released immediately after childbirth)
- A sensation that the fetus is dropping lower into your abdomen (a process called lightening)
- Contractions related to real labor or false labor (also called prodromal labor or Braxton Hicks contractions)
Preparing for childbirth
Being able to spot the early signs of labor (the process of giving birth) and staying mindful of changes in your body are important as you approach your due date. A few of the most common signs that labor is starting include:
- Contractions that are regular and become increasingly strong and frequent. (A contraction is a tightening and then relaxing of the muscles of the uterus that help push the baby out.)
- A dull ache in your lower back that doesn’t go away
- A sudden gush or steady trickle of fluid from your vagina. (This is your “water breaking.”)
- Passing of the mucus plug that was blocking your cervix, which is an indication that the lowest part of your uterus is widening in preparation for childbirth. (A mucus plug may look like clear, brown, or reddish vaginal discharge.)
Contact your HCP immediately if any of these occur, even if you’re several weeks or months away from your due date.
What are the stages of labor?
Labor and childbirth varies from person to person. Your experience may be unlike what family members or friends went through. In general, though, labor can be divided into three stages:
- First stage: This starts with contractions and ends when your cervix (the lowest part of your uterus) has widened to about 4 inches. Typically lasting between 12 and 19 hours, this is the longest stage of labor. Stay in close communication with your HCP as you work through contractions. They’ll let you know when it’s time to prepare for a home birth or head to the hospital or birthing center.
- Second stage: This is known as the active stage. You’ll begin to push your baby out of your vagina by powerfully pressing downward during contractions. This stage usually lasts between 20 minutes and three hours. Once the top of your baby’s head is visible from your vagina (called crowning), your HCP will instruct you when and how long to push to deliver the baby.
- Third stage: Your baby has arrived. The final stage is to give birth to the placenta (sometimes called the afterbirth). This usually begins five to 30 minutes after childbirth and may only take a few minutes.
C-section birth
While most pregnant people give birth through the vagina, around 1 in 3 people in the United States have babies by cesarean section (also called a C-section). This is a surgery to deliver a baby through an incision in the abdomen. Some C-sections are planned, but many are performed when complications arise during labor.
What are the most common pregnancy complications?
Complications during pregnancy can affect the parent, fetus, or both. They may occur in people who are in otherwise good health. Receiving regular prenatal care can help you avoid complications or allow your HCP to promptly identify and address them if they occur.
Some of the most common pregnancy complications include:
Gestational diabetes
Gestational diabetes refers to diabetes that develops in a pregnant person who didn’t have diabetes before pregnancy. Between 2 and 10 percent of pregnancies in the U.S. are affected by gestational diabetes every year, according to the CDC. Around 50 percent of people with gestational diabetes go on to develop type 2 diabetes after pregnancy.
Gestational diabetes occurs when your body can’t produce enough insulin during pregnancy. Insulin is a hormone that helps your body convert blood sugar into energy. Treatment for gestational diabetes involves making healthy lifestyle changes, such as exercising more and eating more healthy foods that won’t cause your blood sugar levels to rise excessively. Insulin injections may also be necessary to help manage blood sugar levels.
Gestational diabetes rarely causes noticeable symptoms. Your HCP will screen for gestational diabetes during prenatal care visits.
Gestational hypertension
Gestational hypertension refers to high blood pressure that develops during pregnancy and does not involve proteins in urine, kidney issues, or additional heart health concerns. It’s often diagnosed after week 20 and usually resolves after childbirth, though people with gestational hypertension may be at a higher risk of experiencing high blood pressure after pregnancy.
Possible signs of gestational hypertension include sudden changes in vision, swelling, headache, nausea, or pain around the upper right side of your abdomen. In some cases, gestational hypertension doesn’t cause any symptoms.
Preeclampsia
Preeclampsia is a type of high blood pressure that can occur suddenly during pregnancy after week 20. It may also lead to excess proteins in urine, kidney issues, liver issues, and serious complications like seizures. Around 1 in 25 pregnant people in the U.S. experience preeclampsia.
In more serious cases of preeclampsia, an HCP may recommend inducing labor (using medication to cause labor to begin) or delivering the baby through a C-section at as early as 34 weeks. Other pregnant people may be advised to remain on bed rest and take medications to lower blood pressure and prevent seizures.
Preeclampsia often resolves on its own after childbirth, though it may also develop shortly after delivery (called postpartum preeclampsia) and last for several days or weeks.
Some cases of preeclampsia don’t cause noticeable symptoms. If symptoms do occur, they may involve:
- A persistent headache
- Sudden changes in vision, such as blurriness or seeing spots
- Vomiting or nausea
- Difficulty breathing
- Upper abdominal pain
- Swelling of the face or hands
- Sudden weight gain
Infections
Routine infections can cause more severe problems for pregnant people. Some infections can spread to a fetus in the womb or pass from parent to baby during childbirth. Examples of infections that could affect a pregnancy include urinary tract infections, influenza (the flu), COVID-19, foodborne illnesses, viral hepatitis, and human immunodeficiency virus (HIV) infection.
You can reduce your risk of infection-related pregnancy complications with appropriate pre-pregnancy and prenatal care. Simple actions like washing your hands thoroughly and receiving routine vaccinations before and during your pregnancy can help you and your baby stay healthy.
Mental health conditions
Mental health conditions like depression are common among pregnant people. A 2020 study published in the Cleveland Clinic Journal of Medicine found that as many as 20 percent of people in the U.S. experience depression during pregnancy (prenatal depression), after pregnancy (postpartum depression), or both (perinatal depression).
Everyone goes through occasional periods of sadness, but depression is different. You may be experiencing depression if your symptoms last for several weeks at a time and interfere with daily life.
Depression symptoms may include:
- Feeling hopeless or unusually pessimistic
- Lingering sadness or emptiness
- Changes in appetite
- Fatigue or loss of motivation
- Sleeping too much or too little
- Irritability or restlessness
- Difficulty focusing, remembering things, or making decisions
- Feeling worthless, ashamed, or guilty
- Thoughts of self-harm or suicide
Anxiety disorders that cause intense worry, fear, nervousness, or panic are also common during and after pregnancy. Contact your HCP right away if you experience signs of anxiety or depression. They may refer you to a mental health provider or prescribe medication to help ease your symptoms.
To receive immediate assistance for severe depression or anxiety symptoms, contact the 988 Suicide & Crisis Lifeline by dialing or texting 988 on your phone. You can also chat with a 988 Lifeline crisis counselor on their website. This service is completely free, confidential, and available 24/7.
Baby blues and postpartum depression
Many people experience “baby blues” after giving birth. Newborn babies require care day and night, which can leave parents feeling exhausted and overwhelmed. Feelings of worry and sadness may occur as a result. Usually, the baby blues are mild and resolve on their own in a few weeks.
Postpartum depression is different. It typically involves more severe symptoms of depression that persist for longer than two weeks after giving birth and that interfere with your daily routine. Reach out to your HCP if you believe you may have postpartum depression. Treatment options are available to help you feel better.
Miscarriage and stillbirth
Miscarriage refers to pregnancy loss that takes place before week 20. Many miscarriages occur before people realize they’re pregnant. Among known pregnancies, between 10 and 20 percent end in miscarriage. Signs of miscarriage may include vaginal bleeding, abdominal cramping, or passing tissue or fluid from the vagina. The causes of most miscarriages are unknown, though chromosomal abnormalities (problems involving genes) are believed to play a role in some cases.
Stillbirth is pregnancy loss that occurs after week 20. It affects around 1 in every 160 pregnancies in the U.S. each year. Some stillbirths occur during childbirth, although most take place during the pregnancy. Possible signs of stillbirth include vaginal bleeding, pain, and no longer feeling the fetus kick or move. Many cases are linked to infections, preeclampsia, and congenital differences, although the causes of some stillbirths are unclear.
This is not a complete list of pregnancy complications. If you notice any unusual symptoms or changes in your body—such as vaginal bleeding, changes in vision, fever, severe abdominal pain, or persistent vomiting—contact your HCP right away.
You should also seek emergency medical care if you or a pregnant person around you experiences a seizure or signs of shock related to blood loss. This might include sudden weakness or faintness, unusually pale skin, cold and clammy hands, or low blood pressure.
What is a high-risk pregnancy?
A high-risk pregnancy is one that involves a greater likelihood of maternal or fetal complications. Some factors that can make a pregnancy “high risk” include:
- Being pregnant with multiples, such as twins or triplets
- Having a preexisting medical condition, such as high blood pressure, diabetes, lupus, heart disease, cancer, or thrombophilia (a tendency to develop blood clots)
- Previously having a complicated pregnancy, miscarriage, or stillbirth
- Being older than 35
- Having a fetus with congenital differences, such as Down syndrome or cystic fibrosis
With appropriate prenatal care, many people with high-risk pregnancies go on to have smooth deliveries and healthy babies. You may require more frequent healthcare visits or be referred to a maternal-fetal medicine specialist (an obstetrician with advanced training in complicated pregnancies) if your pregnancy is considered high-risk.
What if I have trouble getting pregnant?
An inability to get pregnant after one year of trying is called infertility. If you’re experiencing infertility, you’re not alone. The CDC estimates that 19 percent of women and people AFAB between the ages of 15 and 49 with no prior births have trouble getting pregnant.
Infertility can result from a variety of issues that affect women and people AFAB as well as men and people AMAB. Speak with an HCP if you are unable to get pregnant after a year of trying and are generally healthy. If you’re over age 35, consider visiting your HCP after six months of trying.
Several infertility treatments are available to help you have a baby. Your best course of care will depend on what’s causing the infertility, your age, and your overall health.
Treatments and approaches to infertility include medication, in vitro fertilization, and surrogacy. Intrauterine insemination (IUI), which involves inserting sperm directly into the uterus, is another common infertility treatment. Making healthy lifestyle changes such as quitting smoking, drinking less alcohol, exercising, and reducing stress may also help address infertility.
Learn more about pregnancy
Whether you’re curious about pregnancy, wish to become pregnant, or you recently discovered that you’re expecting, the next step is to speak with a healthcare provider. They can provide you with guidance on how to achieve a healthy pregnancy for you and your baby.
For additional information about pregnancy, browse helpful resources from trusted organizations like the Centers for Disease Control and Prevention.
Featured pregnancy articles

American Pregnancy Association. Cleaning and Pregnancy. Accessed March 28, 2024.
American Pregnancy Association. Early Signs of Pregnancy. Accessed March 19, 2024.
Australian Government Department of Health and Aged Care. Toxic Household Products to Avoid During Pregnancy. Pregnancy, Birth & Baby. Last reviewed December 2022.
Centers for Disease Control and Prevention. Gestational Diabetes. Last reviewed December 30, 2022.
Centers for Disease Control and Prevention. Gestational Hypertension. Last reviewed June 19, 2023.
Centers for Disease Control and Prevention. Infertility. Last reviewed April 26, 2023.
Centers for Disease Control and Prevention. Planning for Pregnancy. Last reviewed February 15, 2023.
Centers for Disease Control and Prevention. Pregnancy Complications. Last reviewed February 8, 2023.
Cleveland Clinic. Conception. Last reviewed September 6, 2023.
Cleveland Clinic. Fetal Development. Last reviewed March 19, 2024.
Cleveland Clinic. Pregnancy Tests. Last reviewed November 28, 2022.
Cleveland Clinic. Ultrasound in Pregnancy. Last reviewed September 28, 2022.
Eunice Kennedy Shriver National Institute of Child Health and Human Development. Pregnancy. Accessed March 18, 2024.
March of Dimes. Miscarriage. Last reviewed February 2023.
March of Dimes. Stillbirth. Last reviewed October 2020.
MedlinePlus. Childbirth. Last updated January 2, 2017.
MedlinePlus. Choosing the Right Health Care Provider for Pregnancy and Childbirth. Last reviewed November 21, 2022.
Office of Disease Prevention and Health Promotion. Eat Healthy During Pregnancy: Quick Tips. Last updated May 19, 2023.
Office on Women’s Health. Labor and Birth. Last updated February 22, 2021.
Office on Women’s Health. Prenatal Care. Last updated February 22, 2021.
Office on Women’s Health. Prenatal Care and Tests. Last updated February 22, 2021.
Office on Women’s Health. Stages of Pregnancy. Last updated February 22, 2021.
Salamon M. What Does a Birth Doula Do? Harvard Health Publishing. Published November 22, 2023.
Salem Health. Emergency Symptoms in Pregnancy. Accessed March 22, 2024.
Sobczak A, Taylor L, Solomon S, Ho J, Kemper S, Phillips B, Jacobson K, Castellano C, Ring A, Castellano B, Jacobs RJ. The Effect of Doulas on Maternal and Birth Outcomes: A Scoping Review. Cureus. 2023 May 24;15(5):e39451.
U.S. Food & Drug Administration. Advice About Eating Fish. Last reviewed March 5, 2024.
US Preventive Services Task Force. Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement. JAMA. 2017;317(16):1661–1667.
Van Niel MS, Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020;87(5):273-277.
Yale Medicine. High-Risk Pregnancy. Accessed March 25, 2024.