Substance use disorder
- What is substance use disorder?
- What are the stages of substance use disorder?
- What types of substances are commonly abused?
- What are the types of substance use disorder?
- What are the signs and symptoms of substance use disorder?
- How is substance use disorder diagnosed?
- What causes substance use disorder?
- What are the risk factors for substance use disorder?
- When should you see a healthcare provider?
- How are substance use disorders treated?
- What are the possible complications of substance use disorder?
- Can you prevent substance use disorders?
- What is the outlook for people with substance use disorder?
- Recovery from substance use disorder
- Featured substance use disorder articles
Introduction
Substance use disorder (SUD) is a complex condition in which a person habitually uses alcohol, drugs, or another addictive substance despite negative consequences. SUDs affect more than 48 million people ages 12 and older in the United States. Also known as substance abuse or drug addiction, SUD can lead to strained relationships, problems at work or home, and serious health complications.
Get the facts on substance use disorders, including the most common warning signs and symptoms. Learn what factors increase the risk of SUDs and how getting treatment can help people recover from substance abuse.
What is substance use disorder?
Substance use disorder is an unhealthy pattern of substance use that distorts a person’s thinking and interferes with their life. It’s characterized by intense, uncontrollable cravings for addictive substances like alcohol or drugs. These substances stimulate the reward center of the brain and may temporarily produce calming, euphoric, or pleasurable feelings. (The reward center is the part of the brain that generates feelings of satisfaction in response to certain experiences or types of stimulus.)
Tolerance develops the longer a person uses a substance. This means it takes more and more of that substance to deliver the desired effect. If a person suddenly stops using the substance, uncomfortable withdrawal symptoms may occur for several days or weeks. These symptoms often include nausea, shaking, or anxiety. Withdrawal symptoms occur because the body craves the substance that it has become accustomed to receiving.
A person with substance use disorder may recognize they have an issue but is unable to correct it on their own. Over time, using drugs or drinking alcohol in excess alters the structure and function of the brain. This makes it difficult for the person to stop using the substance unless they receive help.
Substance use disorder may be mild, moderate, or severe. Addiction is the most severe form of the disease. SUD is often accompanied by other mental health conditions, such as anxiety or depression. Alcohol and drug use are responsible for more than 3 million deaths per year globally, according to the World Health Organization.
What are the stages of substance use disorder?
Substance use disorders (notably drug use disorders) tend to progress in four stages:
- Experimental use: This typically involves recreational use with friends. (Recreational refers to the occasional use of a drug without a medical reason for doing so.) The substance may be used simply to defy authority figures such as parents, in the case of children and teenagers.
- Regular use: Someone who uses regularly may miss time at work or school and start to pull away from friends and family. The substance may be used to numb pain or negative feelings. Increased tolerance may develop.
- Risky or problem use: This is characterized by clear behavior changes and little or no motivation to attend or perform in work or school. The user prioritizes the substance above relationships and other interests.
- Addiction: Someone in addiction has lost control of their use, yet they may deny there is a problem. The user feels that daily substance use is necessary to function. Relationships with family or friends may be broken. Legal and financial woes may deepen. Suicidal thoughts may occur.
What types of substances are commonly abused?
A variety of legal and illegal substances can lead to a substance use disorder. These substances include:
Alcohol
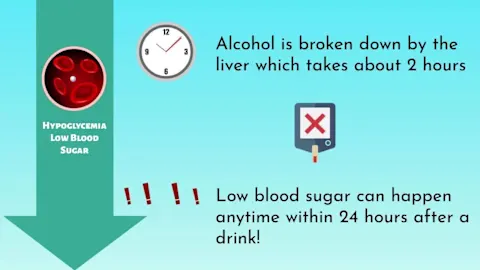
Alcohol use disorder (AUD) begins as alcohol misuse, which involves binge drinking and heavy alcohol use. Heavy alcohol use is defined as binge drinking on five or more days in a month. Binge drinking typically involves consuming about four drinks within a two-hour window, for women and people assigned female at birth (AFAB). For men and people assigned male at birth (AMAB), this happens after about five drinks within that time span. Someone who drinks too much alcohol may have slurred speech, reduced coordination, and lowered judgement.
The Centers for Disease Control Prevention (CDC) advises people of legal age to avoid alcohol or drink it only in moderation. This means men and people AMAB should limit their alcohol consumption to two drinks per day. Women and people AFAB should have no more than one drink per day.
One “drink” is defined as:
- 1.5 ounces of liquor, such as whiskey, gin, vodka, tequila, or rum
- 5 ounces of wine
- 8 ounces of malt liquor, including malt-based seltzers
- 12 ounces of beer
Tobacco and nicotine
Tobacco is a plant that provides the main ingredient for cigarettes, pipes, cigars, dip, and snuff. It contains large amounts of the addictive chemical nicotine. Nicotine is also found in e-cigarettes (vape or vape pens). Someone with nicotine dependence may become anxious, frustrated, angry, or depressed if they can’t satisfy their urge to smoke, vape, or dip.
Depressants
These substances deliver a temporary sense of calm or drowsiness. Side effects of depressant misuse include reduced alertness, increased irritability, poor coordination, and slurred speech.
Depressants include:
- Anxiety medications such as barbiturates (phenobarbital, butalbital, methohexital) and benzodiazepines (alprazolam, diazepam, clonazepam)
- Sedatives and sleep aids such as chloral hydrate and paraldehyde
- Alcohol
Stimulants
Stimulating drugs, which arouse the brain and nervous system, include cocaine, crack cocaine, amphetamines, and methamphetamine. Amphetamines include drugs used to treat attention deficit/hyperactivity disorder (ADHD) and narcolepsy (a type of sleep disorder). Methamphetamine is an illegal street drug known as “meth.”
Stimulants can deliver a “high” that may involve increased energy, heightened alertness, and intense excitement or confidence.
Marijuana
Marijuana is a mind-altering drug that’s derived from the Cannabis sativa plant. It’s also known as cannabis, pot, weed, and dope. Marijuana can cause delayed reaction times, disorientation, and poor coordination.
Recreational use of marijuana is legal or partially legal in many states. Medical marijuana (which may be prescribed by a healthcare provider) is also legal in many states and may be used to help ease chronic pain, nausea, or multiple sclerosis symptoms. It is still a potentially addictive substance, however. Approximately 19.2 million people in the U.S. had a marijuana use disorder in 2023.
Hallucinogens
Substances including lysergic acid diethylamide (LSD or acid), phencyclidine (PCP), mescaline, and psilocybin (“magic mushrooms”) are hallucinogens. This means they cause the user to hallucinate or see things that don’t actually exist. Someone who uses a hallucinogen may also have a diminished sense of reality and display impulsive behaviors.
Opioids
Opioids are powerful painkilling drugs called narcotics. They are typically used to treat severe pain. Opioids such as codeine, morphine, hydrocodone, and oxycodone are prescription narcotics. A type of opioid called heroin is an illegal street drug.
Fentanyl is an especially potent painkiller that’s associated with an increasing number of overdose deaths in the U.S. Illegally made fentanyl may be added to fake prescription drugs or other products sold on the street (including candy) without the buyer’s knowledge.
Substance use disorder involving opioids is known as opioid addiction or opioid use disorder. Misusing opioids may cause symptoms such as drowsiness, slurred speech, agitation, poor memory, and reduced coordination.
Club drugs
Club drugs refer to a group of substances (including several stimulants, depressants, and hallucinogens) that are commonly trafficked at nightclubs and bars. Also known as party drugs, club drugs lower inhibitions and elevate visual and auditory experiences (those associated with seeing and hearing). Common club drugs include LSD, methylenedioxymethamphetamine (also known as MDMA, molly, or ecstasy), ketamine (special K), and GHB (liquid ecstasy).
What are the types of substance use disorder?
Substance use disorder that involves taking a drug is known as a drug use disorder. More than 27 million people in the U.S. had a drug use disorder in 2023. Alcohol use disorder affects an estimated 29 million people in the U.S.
Some people experience multiple substance use disorders at the same time. This may involve using several drugs or combining different types of substances, such as alcohol and opioids. More than 7 million people had both an alcohol use disorder and a drug use disorder in 2023, according to the federal Substance Abuse and Mental Health Services Administration (SAMHSA).
Less commonly, substance use disorders may involve caffeine, substances that are inhaled (inhalants) such as aerosol sprays and paint thinners, and other potentially addictive substances.
What are the signs and symptoms of substance use disorder?
The specific signs and symptoms of a substance use disorder vary based on the substance in question. But all substances can lead to intoxication. This is a state of diminished mental and physical control or altered behavior. Depending on the substance used, intoxication may involve a “high,” sedation, and/or changes in perception.
General symptoms of substance use disorder
In general, someone with substance use disorder may:
- Become angry when questioned about the substance
- Frequently give excuses for using the substance
- Use the substance in secret or when alone
- Spend less time with friends and family
- Have abrupt changes in behavior or mood
- Have violent episodes and display unusually risky behaviors
- Show an unusual lack of care about their physical appearance
- Become confused frequently
- Skip meals or be uninterested in eating
Specific symptoms of substance use disorder
The American Psychological Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) is used by most healthcare providers (HCPs) to diagnose mental health conditions. This manual lists the following substance use disorder symptoms, which generally fall into four main categories:
Impaired control:
- Strong urges or desires to use the substance
- An inability to stop or control substance use
- A significant amount of time spent obtaining, using, or recovering from the substance
Risky usage:
- Substance use in greater amounts or for longer periods than what’s appropriate (this applies to legal substances, such as alcohol and prescribed medications)
- Continued substance use despite harm to relationships or family
- Continued substance use despite harm to physical or mental health
- Continued substance use despite other dangerous consequences
Social issues:
- Less participation in social or recreational activities because of substance use
- Decreased performance at work or school
Drug side effects:
- A growing tolerance to the substance
- Withdrawal symptoms that are reduced by restarting the substance after a period of non-use
How is substance use disorder diagnosed?
An HCP may diagnose a person with substance use disorder if they display at least two of the symptoms listed in the American Psychological Association’s DSM-5-TR (see above).
- Mild substance use disorder is indicated by having two or three symptoms
- Moderate substance use disorder is indicated by having four or five symptoms
- Severe substance use disorder is indicated by having six or more symptoms
An HCP may also evaluate a person’s medical history and perform a physical and psychological exam to check for other signs of substance use disorder. Drug tests (toxicology screens) can also be performed to screen blood or urine samples for evidence of substance use.
What causes substance use disorder?
A complex combination of genetic, behavioral, and environmental factors can lead to substance use disorder. For many people, motivations for using drugs or alcohol involve:
- A desire to numb negative feelings, relieve stress, or forget one’s problems
- Wanting to achieve a “high” or a feeling of pleasure or euphoria
- Wanting to fit in with others
- A desire to enhance thinking or mental or physical performance
Frequent use of substances like drugs and alcohol affects brain structure and function, altering nerve cells and changing how the brain experiences pleasure. This makes it more difficult to quit using the substance without help.
What are the risk factors for substance use disorder?
Having certain risk factors may make someone more likely to develop substance use disorder. These SUD risk factors include:
Age: Substance use disorder is most common in people between the ages of 18 and 25. Use of alcohol or drugs in childhood or adolescence also increases the risk of SUD later in life. Still, SUD can occur at any age and often affects older adults.
Sex assigned at birth: Men and people AMAB are generally more likely to develop substance use disorder than women and people AFAB.
Family history and genetics: Substance use disorder can run in families. A person’s likelihood of SUD increases if they have a parent or sibling with the condition. Researchers have identified several genes that can influence addiction risk. (Genes are units of DNA that are inherited from a person’s parents and help determine their traits.) Genetics are believed to account for 40 to 60 percent of a person’s chances of having a SUD.
Loneliness and isolation: People experiencing loneliness or social isolation have an increased risk of substance use disorder. This trend is evident in older adults who are more likely to lose partners and have fewer social contacts over time. Substance use treatment among adults ages 50 and older has been on the rise in recent decades. A 2021 study of older adults published in Journals of Gerontology found rates of SUD to be highest among those who felt lonely and lived alone.
Adverse childhood experiences: Adults with a history of adverse childhood experiences (ACEs) are more than four times more likely to develop substance use disorder, according to a 2023 study published in Addictive Behaviors Reports. An ACE is an event or series of events that occurs before age 18 and may involve:
- Abuse, violence, or neglect
- Suicide committed or attempted by a family member
- Household instability due to divorce, a jailed family member, or illness (including substance use disorders and mental health conditions)
- Other forms of trauma
The CDC reports that around 64 percent of adults in the U.S. have had at least one type of ACE.
Exposure and access to substances: A person is more likely to use a substance if it’s used by a friend, peer, or member of their household. Someone who is prescribed medication that could be misused, such as fentanyl or amphetamines, can easily access the drug and have more opportunities to become addicted.
It’s important to note that anyone can develop a substance use disorder, even if they don’t have risk factors. On the other hand, many people with multiple SUD risk factors never experience addiction.
Mental health and substance use disorder
Substance use disorders are closely linked to mental health conditions. Around half of people with a mental health condition experience a substance use disorder and vice versa.
Drugs and alcohol are often used to ease the feelings of pain, hopelessness, or worry caused by mental health issues. Similarly, SUD can alter brain function and make someone more prone to mental health conditions.
Mental health conditions that are commonly associated with SUD include:
When should you see a healthcare provider?
Contact an HCP such as a primary care provider or a licensed mental health provider if you or someone you know has substance use disorder and needs help. If this provider doesn’t treat SUD, they can refer you to an HCP who does.
You can also contact SAMSHA’s National Helpline to be referred to a treatment provider in your area. The sooner a person receives care for substance abuse, the greater their odds of long-term recovery.
It's particularly important to speak with an HCP if you or a loved one:
- Are unable to stop using a substance, even when it causes harm
- Are at risk of withdrawal (for example, you’ve been cut off from your drug supply) or may be experiencing withdrawal symptoms
- Engage in risky behaviors such as having unprotected sex or sharing drug equipment
Coping with substance use disorder may lead to suicidal thoughts or behaviors. If you or someone you know needs immediate assistance for a mental health concern, call 911 or contact the 988 Suicide & Crisis Lifeline by calling or texting 988. You can also chat with a provider online. The 988 Lifeline is completely confidential, free, and available 24/7/365.
When to call 911
Substance use disorder can lead to health complications that warrant emergency medical care. Call 911 immediately if you or someone around you experiences:
- Trouble breathing
- Reduced consciousness or loss of consciousness
- Confusion
- Signs of a heart attack, including chest pain or pressure
- Convulsions or seizures
- Thoughts of suicide
- Other distressing physical or psychological issues
What to do if a loved one needs help
Many people with substance use disorder are hesitant to accept help or admit they have a problem. When encouraging a loved one to seek help for substance abuse, make it clear that you care for them and are there to support them. (This process is sometimes called an intervention.)
Discuss the potential consequences of continued substance use and the benefits of treatment. Reference specific concerning behaviors they display rather than placing a label on the issue (such as “alcoholism”) or assigning the person a label (such as “alcoholic”).
As you speak with your loved one, try to avoid lecturing, threatening, or begging them to seek help. Be open and honest, but understand that the person has a legitimate illness that requires professional care. Don’t confront a loved one when they’re intoxicated and unable to hold a rational conversation.
Involving an HCP in the intervention may also be beneficial. They can provide you with guidance about approaching your loved one or help direct the intervention themselves. Speak with your HCP to learn more or ask them to refer you to an intervention specialist for further assistance.
How are substance use disorders treated?
Substance use disorder is a disease that affects many aspects of life. Because of this, the best approach is often one that involves several types of treatment that are tailored to the individual. The overall goal of substance use treatment is to achieve abstinence, or a life without substance use.
Substance use disorder treatment settings
Treatment may be provided in a variety of settings depending on the type and severity of the substance use disorder. These treatment settings include:
- Outpatient: The patient receives treatment while living at home and visiting the treatment facility as needed.
- Intensive outpatient: The patient lives at home and attends therapy sessions several times per week.
- Inpatient: The patient lives and receives treatment at a residential treatment center (also called a rehabilitation or “rehab” center). Many inpatient treatment centers are staffed with HCPs and mental health providers who specialize in treating substance use.
- Therapeutic community: The patient lives in a highly controlled, drug-free environment (such as a sober living community or sober house) for an extended period of time.
An individual’s SUD treatment plan will likely include a combination of approaches, including:
Detoxification
Detoxification (or “detox”) is often the first step of substance use disorder treatment. It involves stopping substance use under the guidance of an HCP, either in an outpatient or inpatient setting.
Someone who is detoxing from a substance will likely experience withdrawal symptoms. These can range from mild to severe and may include:
- Chills
- Headaches
- Insomnia
- Rapid heart rate
- Vomiting
- Diarrhea
- Seizures
More severe withdrawal symptoms may need to be managed in a hospital. Psychological symptoms, such as mood swings, anxiety, and depression, may also occur.
The time it takes to detox from a substance will depend on the substance in question and the severity of the disorder. Withdrawal symptoms are typically worst in the first few days of detox, then gradually improve. Medication may be provided to ease withdrawal symptoms and cravings during detox.
Medication
When combined with therapy, medication can help reduce cravings and prevent relapses (return to substance use) in people with substance use disorder.
The U.S. Food and Drug Administration (FDA) has approved several medications that assist people with alcohol and opioid use disorders.
Medications for alcohol use disorder include:
- Disulfiram, which causes unpleasant physical reactions if alcohol is consumed
- Naltrexone, which blocks the euphoric effect of alcohol
- Acamprosate, which reduces cravings
Medications for opioid use disorder include:
- Naltrexone, which blocks the euphoric effect of opioids
- Methadone, which reduces cravings and withdrawal symptoms
- Buprenorphine, which also reduces cravings and withdrawal symptoms
Medications are also available to help people quit smoking and using other forms of tobacco. These include smoking cessation drugs such as varenicline and bupropion. Nicotine replacement therapies, such as nicotine patches, sprays, lozenges, or gums, may also ease smoking or vaping cravings.
Counseling and behavioral therapy
Speaking with a mental health provider such as a counselor, clinical social worker, psychologist, or psychiatrist is an important part of substance use recovery. These professionals can help a person:
- Acknowledge the presence of the disorder
- Identify unhealthy and detrimental thinking patterns
- Understand how thoughts influence behavior and contribute to substance use
- Learn healthier habits and thinking patterns
- Increase mindfulness and acceptance of the present, which can help ease depression and reduce cravings
- Adopt healthy coping mechanisms to reduce dependence on drugs and alcohol
Since substance use disorders and mental health conditions commonly occur alongside each other, many people also receive therapy for mental health concerns during substance use recovery. There are several types of behavioral therapies that can help people with substance use and mental health issues, including:
- Cognitive behavioral therapy (CBT): A of talk therapy that uncovers unhealthy thinking patterns and teaches positive coping mechanisms
- Dialectical behavioral therapy (DBT): A mindfulness-based approach that focuses on accepting the present, managing difficult emotions, and improving relationships
- Contingency management (CM): An incentive-based therapy that rewards the patient for displaying healthy behaviors and reaching measurable goals
Support groups and group therapy for substance use disorder
Many people with substance use disorder benefit from attending support groups or group therapy. These online or in-person gatherings allow people who face similar challenges to connect, share stories, and provide encouragement.
Support groups and group therapy offer many of the same benefits, but they differ slightly. Group therapy is led by a mental health provider and involves structured, guided discussions. A support group, which can be led by a peer or a mental health provider, is typically less structured and focuses on providing a sense of belonging and understanding among participants.
Speak with your HCP or mental health provider to learn more about support groups, group therapy sessions, and the type of group that may be right for you. You can also browse support groups led by organizations such as:
- Narcotics Anonymous (NA)
- Alcoholics Anonymous (AA)
- Al-Anon (AA with family participation)
- National Alliance on Mental Illness
- SMART Recovery
Complementary approaches
When combined with traditional treatments for substance use disorder, complementary therapies may help some people cope with the ups and downs of treatment and achieve a sense of balance or control. Complementary therapies tend to be alternative, drug-free approaches.
Examples of complementary approaches for substance use disorder include:
- Yoga
- Qigong
- Acupuncture
- Mindfulness meditation
- Music therapy
- Massage therapy
- Hypnotherapy
- Biofeedback (which helps the patient regulate body functions such as breathing and heart rate)
Ask your HCP about the complementary approaches that may be beneficial for you.
What are the possible complications of substance use disorder?
Substance use disorder is a dangerous disease that can affect multiple parts of the body, including the brain, heart, liver, immune system, and more. The disorder may strain relationships, increase the risk of accidents, and result in financial and legal woes.
SUD can cause a wide range of health complications, including but not limited to:
- Depression, anxiety, and other mental health conditions
- Forgetfulness, memory loss, poor concentration, and other cognitive issues
- Viral infections like HIV, hepatitis B, or hepatitis C from shared use of drug equipment
- Sexually transmitted infections or unwanted pregnancies due to impaired judgement and unsafe sexual practices
- Stroke
- Heart failure and other forms of heart disease
- Liver disease and failure
- Cancers related to alcohol use disorder, such as esophageal cancer, stomach cancer, breast cancer, liver cancer, and colon cancer
- Dental health issues
- Pregnancy complications
- Brain damage
Drug and alcohol overdose
An overdose occurs when a person consumes a toxic and potentially deadly amount of a substance. Overdoses are the most common injury-related cause of death in the U.S., according to the CDC. Opioids—namely, illegally made fentanyl—make up the majority of overdose deaths.
A 2023 study published in the CDC’s Morbidity and Mortality Weekly Report examined overdose deaths in 29 states and the District of Columbia. The study found that overdose deaths involving counterfeit (illegally manufactured or prescribed) pills more than doubled between July 2019 and December 2021. In states in the western U.S., overdose deaths more than tripled.
These counterfeit drugs are often made with deadly doses of illegal fentanyl or benzodiazepines. You can help prevent counterfeit pill overdose by only taking pills prescribed by your HCP.
Signs of an overdose
Call 911 immediately if someone around you displays signs of an alcohol or drug overdose. If possible, position the person on their side to prevent them from choking if vomiting occurs.
Signs of an overdose may include:
- Unresponsiveness or loss of consciousness
- Dizziness, drowsiness, or confusion
- Nausea and vomiting
- Gurgling or choking sounds
- Unusually pale or clammy skin
- Labored or shallow breathing
- Slow or rapid pulse
- Bluish lips or fingernails
- Hallucinations or visual disturbances
- Seizures
Treatment for an overdose will depend on the substance (or substances) that caused the overdose. Naloxone, a medication available as an injection or nasal spray, can help reverse opioid overdose when administered shortly after symptoms begin. Consider keeping naloxone on hand and learn how to administer the medication if you live with someone with opioid use disorder.
Can you prevent substance use disorders?
Substance use disorder is preventable with education. Drug education in schools, communities, and homes can help stop SUD before it starts. The best way to prevent SUD at any age is to avoid using or experimenting with drugs or alcohol.
If your HCP prescribes a potentially addictive medication (such as an opioid or sedative), use it exactly as prescribed. Store medication in a safe place away from children. Never take more medication than instructed and promptly dispose of any leftover pills once treatment is complete.
Parents and guardians can also help prevent substance use in their children by setting a good example and encouraging open communication about difficult subjects like peer pressure and drug use. The risk of substance use disorder is higher in children with family members who misuse alcohol and drugs. Avoiding these risky behaviors can help your child do the same.
What is the outlook for people with substance use disorder?
Substance use disorder is a chronic, lifelong condition. But recovery is possible. Many people with SUD are able to change their behaviors and overcome addiction with comprehensive treatment, ongoing support, and a lasting commitment to abstinence.
In 2023, among the 30.5 million adults in the U.S. who claimed they ever had a substance use issue, more than 73 percent considered themselves recovered or in recovery.
A person’s substance use disorder prognosis (expected outcome) will depend on several factors, including:
- The substance or substances being used
- The severity of the disorder
- The level of commitment to recovery
- Genetics and environment
Relapses are fairly common in substance use recovery. Between 40 and 60 percent of people who receive treatment for substance use disorder will relapse within one year. Continued treatment can help people recover from relapses and achieve their goals.
Recovery from substance use disorder
Substance use disorder is a real disease, not a moral failure or lack of self-control. It affects people of all sexes, genders, races, ethnicities, backgrounds, and income levels. Many people with the condition face stigma that can cause shame, reinforce unhealthy behaviors, and create barriers to treatment. Just 1 in 4 people classified as needing SUD treatment received help in 2023, according to SAMHSA.
If you’re recovering from substance use disorder, it’s important to remember that you’re one of tens of millions in the U.S. With treatment and determination, you can overcome substance abuse. Following these tips can help you stay on track:
- Steer clear of high-risk situations. This may include areas of town where you used to purchase or use substances or groups of people who encourage or participate in substance abuse.
- Stick to your treatment plan. Even if you consider yourself recovered, continue to follow your treatment plan and seek help if you feel tempted. Ongoing participation in therapy and support groups can help you stay sober.
- Immediately get help if you relapse. Contact your HCP right away if you start using substances again. Relapses are common, but treatment can put you back on the path to recovery.
Reach out to an HCP if you or someone you know needs help for substance use disorder. To learn more about the signs of substance abuse and how you can help a loved one, seek resources from these organizations:
Featured substance use disorder articles

American Academy of Family Physicians. Club Drug Use. Familydoctor.org. Last updated June 2022.
American Psychiatric Association. What is a Substance Use Disorder? Last reviewed April 2024.
Deibler M. Understanding Group Therapy and Support Groups. Anxiety & Depression Association of America. Published August 31, 2022.
BetterHealth Channel. Drug Overdose. Last reviewed December 22, 2023.
Broekhof R, Nordahl HM, Tanum L, Selvik SG. Adverse childhood experiences and their association with substance use disorders in adulthood: A general population study (Young-HUNT). Addict Behav Rep. 2023;17:100488. Published 2023 Mar 30.
Centers for Disease Control and Prevention. About Adverse Childhood Experiences. Last reviewed May 16, 2024.
Centers for Disease Control and Prevention. About Standard Drink Sizes. Last reviewed May 15, 2024.
Centers for Disease Control and Prevention. National Center on Health Statistics – Provisional Drug Overdose Death Counts. Last reviewed August 14, 2024.
Centers for Disease Control and Prevention. Preventing Opioid Overdose. Last reviewed May 8, 2024.
Centers for Disease Control and Prevention. Treatment of Substance Use Disorders. Last reviewed April 25, 2024.
Cleveland Clinic. Marijuana (Cannabis, Weed). Last reviewed November 5, 2023.
Cleveland Clinic. Substance Use Disorder (SUD). Last reviewed October 20, 2022.
Common Comorbidities with Substance Use Disorders Research Report. Bethesda (MD): National Institutes on Drug Abuse (US); 2020 Apr.
Farmer AY, Wang Y, Peterson NA, Borys S, Hallcom DK. Social Isolation Profiles and Older Adult Substance Use: A Latent Profile Analysis, The Journals of Gerontology: Series B, Volume 77, Issue 5, May 2022, Pages 919–929,Learn.Genetics. Genes and Addiction. Accessed September 5, 2024.
Mayo Clinic. Drug Addiction (Substance Use Disorder). Last reviewed October 4, 2022.
MedlinePlus. Substance Use Disorder. Last reviewed April 30, 2022.
National Institute on Drug Abuse. Opioids. Last reviewed March 2024.
National Institute on Drug Abuse. Stigma and Discrimination. Last reviewed June 2022.
National Institute on Mental Health. Substance Use and Co-Occurring Mental Disorders. Last revised March 2024.
O’Donnell J, Tanz LJ, Miller KD, et al. Drug Overdose Deaths with Evidence of Counterfeit Pill Use — United States, July 2019–December 2021. MMWR Morb Mortal Wkly Rep 2023;72:949–956.
Slomski A. Mindfulness-Based Intervention and Substance Abuse Relapse. JAMA. 2014;311(24):2472.
Substance Abuse and Mental Health Services Administration. 2023 National Survey on Drug Use and Health (NSDUH) Releases. Accessed September 3, 2024.
Substance Abuse and Mental Health Services Administration. Medications for Substance Use https://www.mdpi.com/2076-328X/11/10/133 Disorders. Last updated April 11, 2024.
U.S. Department of Veterans Affairs. Substance Use Disorder Treatment: Complementary Approaches. Last updated March 10, 2022.
Volkow N. Older Black Men are Disproportionately Affected by the Overdose Crisis. National Institute on Drug Abuse. Published August 30, 2024.
World Health Organization. Over 3 Million Annual Deaths Due to Alcohol and Drug Use, Majority Among Men. Published June 25, 2024.