5 terms for people with eosinophilic asthma to understand
Learn about eosinophils, biologic therapies, and other key terms pertaining to e-asthma.
Updated on March 31, 2025

Roughly 28 million people in the United States. have asthma, a chronic condition of the respiratory system that makes it difficult to breathe. A person having an asthma attack usually experiences coughing, wheezing, and a sense of breathlessness, and in severe cases, will have severe difficulty breathing.
There are several different subtypes of asthma, one of which… Show More
Roughly 28 million people in the United States. have asthma, a chronic condition of the respiratory system that makes it difficult to breathe. A person having an asthma attack usually experiences coughing, wheezing, and a sense of breathlessness, and in severe cases, will have severe difficulty breathing.
There are several different subtypes of asthma, one of which is eosinophilic asthma, or e-asthma. This type of asthma is related to high levels of a white blood cell called eosinophils. Here are several important terms related to e-asthma, as well as a rare disease that is associated with asthma symptoms and very high levels of eosinophils.
Show Less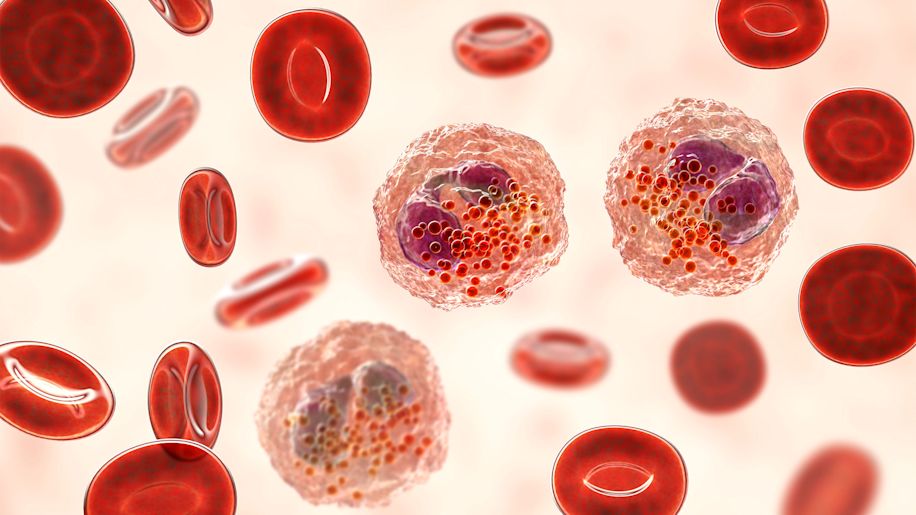
Eosinophils
Eosinophils are a type of white blood cell that play an important role in the body’s immunological response, helping to protect against things like infectious bacteria and parasites. Abnormally high levels of eosinophils are linked to several disorders and health conditions, including most cases of… Show More
Eosinophils are a type of white blood cell that play an important role in the body’s immunological response, helping to protect against things like infectious bacteria and parasites. Abnormally high levels of eosinophils are linked to several disorders and health conditions, including most cases of asthma.
In people who have e-asthma, eosinophils levels are high, leading to inflammation and narrowed airways. Your healthcare provider (HCP) will determine your eosinophil levels using a blood test, but may also examine a sputum (mucus from the lungs) sample. In some instances, an HCP may order a bronchial biopsy, during which a tissue sample is taken from the airways and tested in a lab for the presence of eosinophils. Because this test is more invasive, it is not typically used during an initial diagnosis.
Show Less
“Difficult-to-Control”
You may hear an HCP describe your asthma as “difficult-to-control,” “difficult-to-treat,” “therapy-resistant,” or simply “difficult asthma.” These terms are used to describe asthma that is not well controlled, even when using high-dose controller medications.
When a person has difficult-to-… Show More
You may hear an HCP describe your asthma as “difficult-to-control,” “difficult-to-treat,” “therapy-resistant,” or simply “difficult asthma.” These terms are used to describe asthma that is not well controlled, even when using high-dose controller medications.
When a person has difficult-to-control asthma, they will work with their HCP to identify weak points in their treatment plan that may be preventing the asthma from being controlled. This can include everything from correcting inhaler technique to finding and eliminating asthma triggers. It can also include making lifestyle changes that can improve asthma control, such as quitting smoking and losing weight. An HCP will also look for other health conditions that may be causing the symptoms, such as gastroesophageal reflux disease (GERD), chronic obstructive pulmonary disease (COPD), or vocal cord dysfunction.
Show Less
Severe asthma
Some people with difficult-to-control asthma have severe asthma. E-asthma is a type of often-severe asthma. There are a few ways of categorizing asthma severity. One is based on the frequency of symptoms, lung function, how much asthma interferes with normal activities, and how often asthma… Show More
Some people with difficult-to-control asthma have severe asthma. E-asthma is a type of often-severe asthma. There are a few ways of categorizing asthma severity. One is based on the frequency of symptoms, lung function, how much asthma interferes with normal activities, and how often asthma interferes with sleep. Another is based on the type of treatment required to control the asthma. Severe asthma requires treatment with higher-dose inhaled corticosteroids or oral corticosteroids and long-acting bronchodilators. However, some people with severe asthma are unable to get symptoms under control, even with these treatments.
Show Less
Biologic therapy
Some people are unable to achieve control over severe asthma symptoms, even when treating with traditional types of controller medications. If this is the case, your HCP may recommend treating asthma with what is called a biologic therapy. Biologic therapies are also called immunomodulators. They… Show More
Some people are unable to achieve control over severe asthma symptoms, even when treating with traditional types of controller medications. If this is the case, your HCP may recommend treating asthma with what is called a biologic therapy. Biologic therapies are also called immunomodulators. They modulate (control or modify) how the immune system works in order to reduce symptoms. In the case of e-asthma, an immunomodulator would reduce the amount of eosinophils causing inflammation.
There are several varieties of immunomodulators used to treat asthma. Some are specifically used for eosinophilic asthma, while others are used for non-eosinophilic severe asthma. These medicines are usually taken by injection, and some can be self-administered after training by an HCP. These medications are not used to treat asthma attacks and are typically used as add-on therapies with other forms of asthma treatments.
Show Less
EGPA or Churg-Strauss Syndrome
EGPA stands for eosinophilic granulomatosis with polyangiitis. It is formerly known as Churg-Strauss syndrome, and that term still appears in some of the literature around eosinophilic diseases.
If you’re researching eosinophilic asthma, you may come across a mention of this rare autoimmune… Show More
EGPA stands for eosinophilic granulomatosis with polyangiitis. It is formerly known as Churg-Strauss syndrome, and that term still appears in some of the literature around eosinophilic diseases.
If you’re researching eosinophilic asthma, you may come across a mention of this rare autoimmune disease, which is also related to very high levels of eosinophils. EGPA causes inflammation of the blood vessels throughout the body including the lungs, nerves, skin, and GI tract. When these vessels become inflamed, it can hamper blood flow to the organs and tissue. Some people some experience only a mild case, while others have full-blown symptoms and complications. Most people with EGPA first develop symptoms between the ages of 30 and 50. Asthma, allergies, sinusitis, and pneumonia, or a worsening of existing symptoms, are usually the first signs of the disease. As the disease progresses, it can affect the lungs, gastrointestinal tract, nerves, heart, and blood vessels, and damage many different areas of the body.
Show Less
Apfed.org. Eosinophilic Asthma. March 2020.
Centers for Disease Control and Prevention. NHIS Child Summary Health Statistics. July 22, 2024.
Centers for Disease Control and Prevention. NHIS Adult Summary Health Statistics. July 22, 2024.
Asthma and Allergy Foundation of America. Asthma Facts and Figures. September 2024.
American Lung Association. What Is Asthma? October 23, 2024.
MedlinePlus. Eosinophilic Disorders. March 29, 2017.
Cincinnati Children’s. What is an Eosinophil? Accessed March 31, 2025.
Merck Manual Consumer Version. Asthma. December 2023.
Mayo Clinic. Eosinophilia. September 8, 2023.
Asthma + Lung UK. Types of Asthma. June 30, 2024.
Yılmaz İ. Confusing Terminology: Difficult Asthma, Difficult-to-Treat Asthma, Difficult-to-Control Asthma, Therapy-Resistant Asthma, Severe Asthma, and Refractory Asthma. Which One is Truly Severe Asthma? Turk Thorac J. 2018 Sep 13;19(4):235-236.
GINA. Difficult-to-treat & severe asthma in adolescent and adult patients. November 2018.
Merck Manual Consumer Version. Drugs for Preventing and Treating Asthma. September 2023.
American Academy of Allergy Asthma & Immunology. Immunomodulator Allergy Medications. January 2024.
Chung KF, Wenzel SE, Brozek JL, Bush A, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014 Feb;43(2):343-73.
Apfed.org. Eosinophilic Granulomatosis with Polyangiitis. March 2020.
Mayo Clinic. Churg-Strauss syndrome. February 7, 2024.
American Academy of Allergy Asthma & Immunology. Churg-Strauss Syndrome Overview. June 10, 2024.
Merck Manual Consumer Version. Eosinophilic Granulomatosis with Polyangiitis. January 2025.
Featured Content


video
