Updated on November 13, 2024
Atopic dermatitis (AD), also called eczema, is a chronic condition that causes dry, irritated, itchy patches on the skin. It affects about 10 percent of people in the United States. Around 7 percent of adults and nearly 11 percent of children have some form of the condition.
Atopic dermatitis can have a severe impact on a person’s quality of life. That’s partly due to the uncomfortable symptoms. It’s also because, in addition to skin problems, people with AD are at a higher risk for many other health issues.
Health issues linked to AD
Studies have found that AD is associated with a higher risk of developing the following diseases and conditions.
- Asthma
- Food allergies and sensitivities
- Eye problems including conjunctivitis (pink eye), dry eye, and blepharitis (inflammation of the eyelids)
- Skin issues like alopecia areata (loss of hair in patches) and vitiligo (loss of skin color in patches)
- Autoimmune diseases like inflammatory bowel disease, lupus, and rheumatoid arthritis
- Greater risk of infection
- Osteoporosis, or loss of bone density
- Depression
- Anxiety
Many experts believe there may be a link between AD and cancer, heart disease, and diabetes. But research is relatively limited. And in some cases, studies have shown mixed results.
Why the risk is higher for people with AD
Some of the increased risk for health issues is due to the inflammation associated with AD. Inflammation plays a large role in a wide variety of diseases and conditions.
Another reason for the increased risk: some of the medications used to treat AD. Though they’re helpful for reducing AD symptoms, they can harm other parts of the body, especially if they’re used for too long. For example, systemic corticosteroids reduce inflammation but can also contribute to osteoporosis. That said, it’s crucial to never stop taking a medication without speaking with your HCP first. Doing so can exacerbate AD symptoms and cause additional problems.
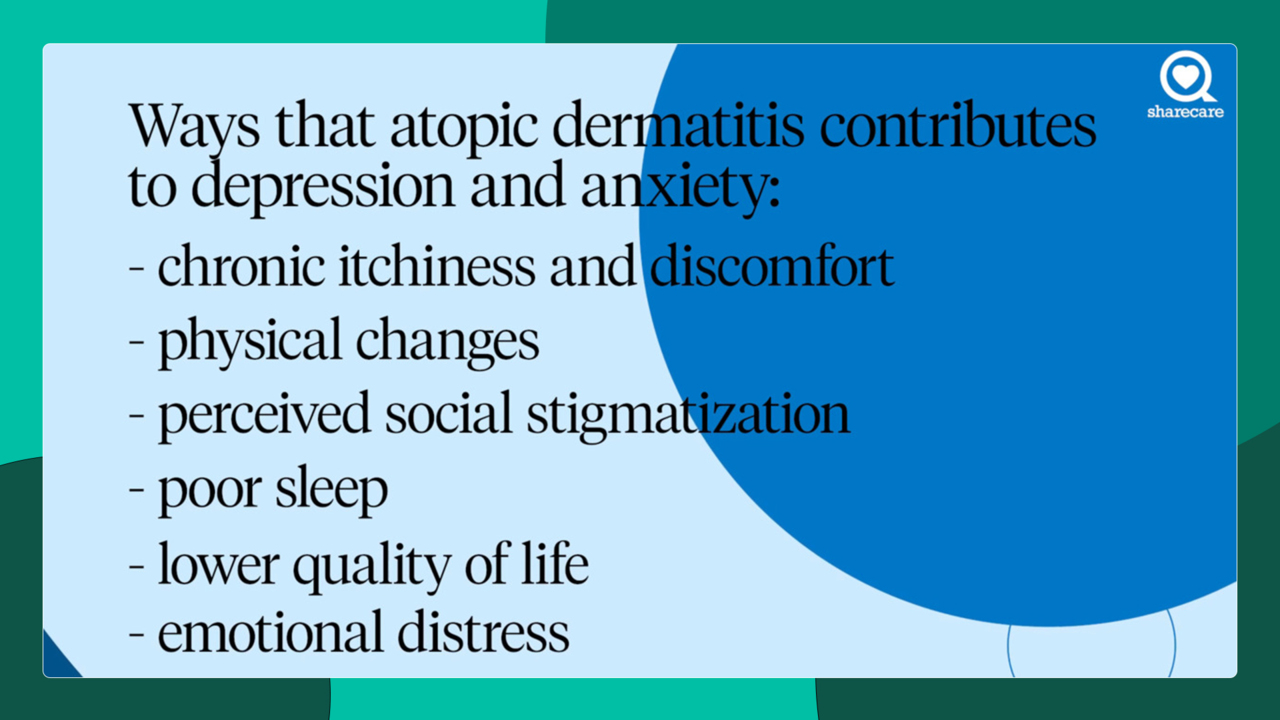
Another explanation may be the toll that AD takes on a person’s emotional wellbeing and mental health. Having a skin condition is stressful. A person with AD may feel self-conscious about their appearance, frustrated when flare-ups persist, or worn out by the never-ending skincare routine. These can contribute to depression and anxiety, which in turn, can play a role in other health issues. For example, people with depression may more likely to smoke or skip appointments with a healthcare provider.
What you can do to help
There’s no cure for AD. But there are many steps you can take to reduce your risk of developing other health issues.
An important first step is working with your healthcare provider (HCP) to come up with an AD treatment plan that works for you. Controlling AD symptoms and reducing flare-ups can help lower stress levels, improve the quality of your sleep, and free up energy that you can direct into improving your overall health.
Adopting these habits can also make a difference:
- Make time for regular physical activity.
- Eat a healthy diet consisting largely of fruits, vegetables, whole grains, legumes, low-fat dairy, and lean protein like chicken and fish.
- Reduce your intake of added salt, sugar, and saturated fat by reducing the amount of processed foods you eat.
- If you smoke, quit,
- Limit your alcohol consumption.
Speak with your HCP for more recommendations.