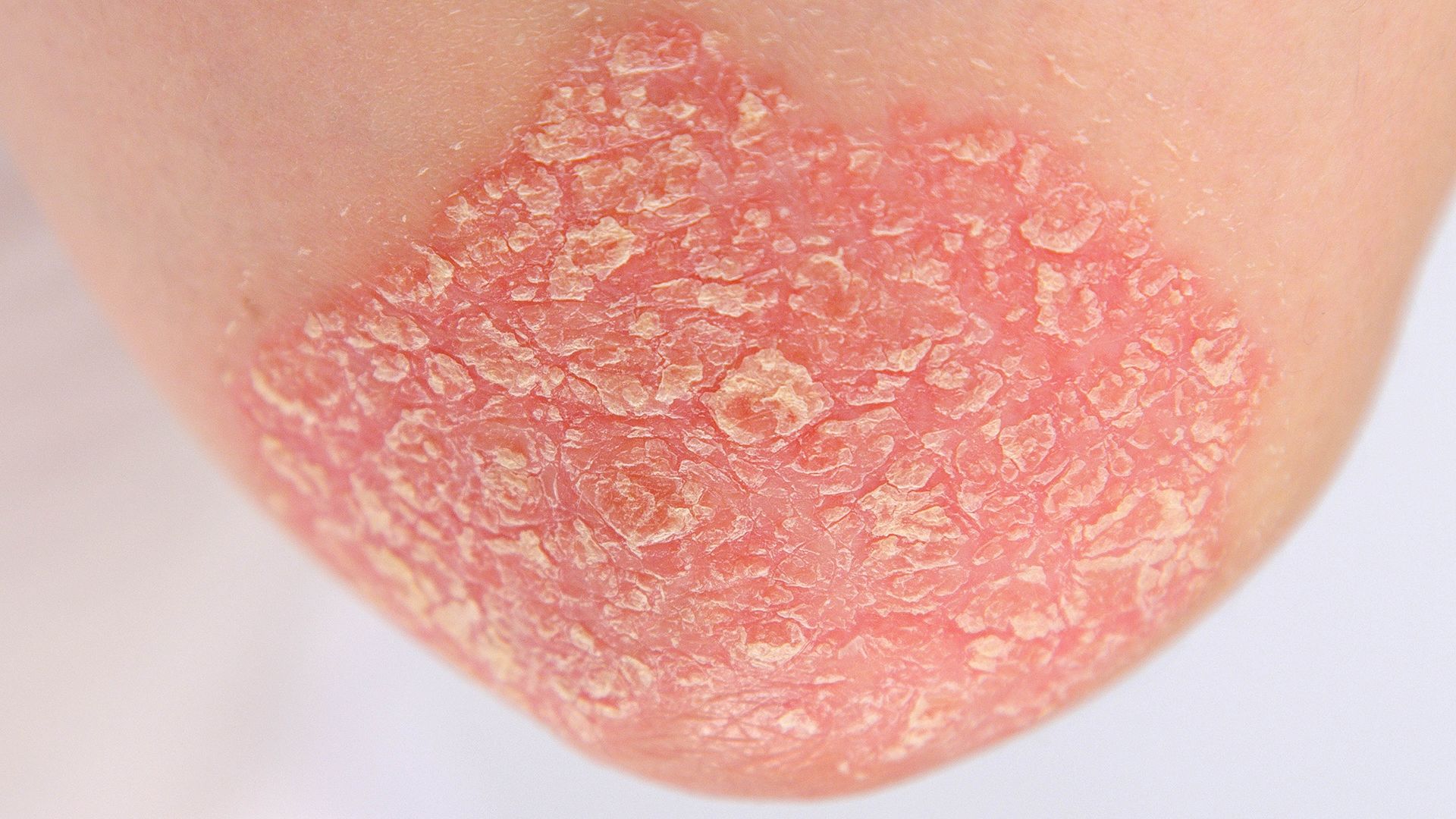
Plaque psoriasis is an autoimmune disease that causes scaly patches of dead skin cells, called plaques. These painful, itchy patches can appear anywhere on the body, but most often appear on the elbows, knees, lower back and scalp.
There’s currently no cure for plaque psoriasis, so treatment focuses on relieving symptoms, reducing the amount of psoriasis on your body and ultimately achieving clear skin.
Topical treatments and light therapy
If you’ve been diagnosed with plaque psoriasis, you probably know a bit about topical treatments, or medicines that are applied directly to the skin. Topical treatments include everything from over-the-counter moisturizers that you apply after every shower, to corticosteroids that are applied to affected areas during flares.
Topical treatments are usually the first line of treatment for plaque psoriasis, and are sometimes used along with light therapy (also called phototherapy). Light therapy involves exposing the skin to natural sunlight or artificial UV light. This treatment should always be done under the guidance of a healthcare provider, as UV light needs to be directed only at the affected areas and too much UV light can damage the skin and make symptoms worse.
If this approach does not improve symptoms or stops working, it’s time to see your healthcare provider to talk about other treatment options.
Here are some of the topics and questions you might expect to discuss during your appointment:
What other treatment options are available?
If topical treatments and light therapy are unsuccessful or stop working, your healthcare provider may discuss systemic and biologic treatments.
- Systemic treatments suppress immune system activity in order to prevent the autoimmune responses that trigger the growth of psoriasis plaques. There are several different types available, and they can be taken as a pill or as an injection.
- Biologics are genetically engineered drugs made from living cells. While systemic drugs work on the entire immune system, biologics target specific cells and proteins within the immune system in order to stop the autoimmune responses that trigger the growth of psoriasis plaques. Biologics are given as an injection (which can sometimes be taken at home) or an intravenous infusion taken at the office of a healthcare provider.
What could be triggering flare-ups?
Another approach to treatment is identifying and avoiding triggers—the things that cause psoriasis flares. When you get to your doctor appointment, be prepared to discuss the products you’re using, including moisturizers, makeup, shampoos, soaps, dish detergents, prescription medications, over-the-counter medicines and any dietary supplements you take. Ingredients in any of these might exacerbate symptoms, and certain over-the-counter medicines and supplements can affect how a treatment works.
What other changes can I make?
Your healthcare provider may also discuss lifestyle changes that might help in managing plaque psoriasis, such as losing weight, cutting back on alcohol, quitting smoking, exercising, eating a healthier diet and reducing stress. Tobacco, alcohol, excess bodyweight and stress are all correlated with more severe psoriasis symptoms.
Don’t give up!
Research has shown that psoriasis often goes untreated or undertreated.
Finding an effective treatment for plaque psoriasis can be tricky and frustrating, and may take some time. Many people with plaque psoriasis cycle through a number of treatments before finding one that works, while others see treatments work well at first, but become less effective with time, or stop working altogether. Patients may also need to change treatments if they are experiencing side effects.
Know your treatment options, keep track of your symptoms and talk to your healthcare provider. It’s important to give new treatments a chance to work. Don’t give up on finding a treatment that works for you.