Ten surprising facts about menopause
Learn about hair differences, foggy thinking, and other changes.
Updated on January 9, 2024

Menopause is a natural life transition that can raise a range of emotions, questions, and concerns, and not everyone talks about it.
"I wish more women knew that what they’re feeling is normal," says Afua Mintah, MD, an OBGYN at St. Mary Medical Center in Langhorne, Pennsylvania. "Many women just need validation that these experiences aren’t in their head, and they’re not being imagined."
With that in mind, here are 10 surprising facts about menopause, along with tips to help ease the transition.
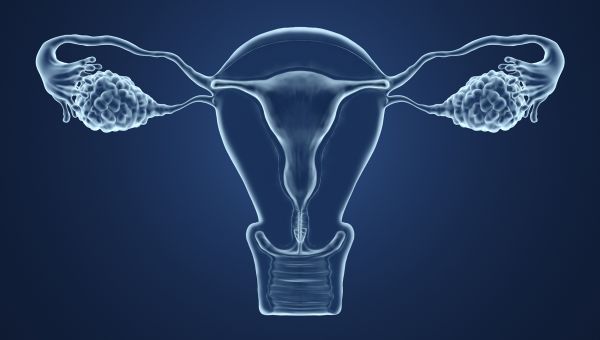
Your Vagina And Vulva May Change
Estrogen contributes to the development of female sex traits like breasts and changes in the uterine lining throughout the menstrual cycle, along with regulation of certain bodily functions like menstruation and sleep. During menopause, estrogen levels decrease, which can lead to a common condition called genitourinary syndrome of menopause (GSM). People with GSM experience a range of uncomfortable symptoms in the vulva and vagina, as well as issues with the urethra, bladder, and labia.
“Without estrogen, the walls of the vagina become thin and dry,” says Dr. Mintah. This can cause pain during sex by making the vagina more prone to irritation and tiny tears. You may also develop itching, burning, and dryness in your vulva and vagina.
“Additionally, decreased collagen reduces the elasticity of vaginal tissues and can make the entire vagina shorter and narrower,” adds Mintah. Prior to menopause, the vagina has more folds, allowing it to stretch easily during intercourse. When the vagina shortens and loses some of those folds, it becomes more difficult to accommodate penetration during sex. The vulva can lose elasticity, as well.
You may also experience light bleeding or spotting after sex. While this is typical, it’s important to understand that it could indicate a more serious condition, such as cervical cancer. If you bleed after sex, speak with a healthcare provider (HCP).

Vaginal Estrogen Is An Option
So, how can you ease GSM symptoms?
Some people take oral pills to address menopause symptoms like hot flashes in addition to GSM. But for GSM only, vaginal estrogen is a first-line treatment—a prescription medication used to address symptoms like burning and dryness. It comes in multiple forms, including extended-release inserts, tablets, liquid-filled capsules, creams, and rings. Unlike medication taken orally, these products are inserted into the vagina. The result is a lower amount of estrogen in your bloodstream than you would receive from an oral treatment. Your HCP can help decide which product might work best for you.
To note: People who use vaginal estrogen do not need to take progestogen, whether or not they still have a uterus.

Consider Lube
If you experience discomfort during sex, there are more solutions and treatment options than you might think. "Lubricants, for one thing, are inexpensive and readily available," says Mintah.
"Applied to the vagina or vulva, lubricants aren’t absorbed into the skin, but rather act on the surface to decrease friction. Use them liberally if dryness is interfering with your ability to stay sexually active," she says. Not sure which is right for you?
Use water-based lubricants like KY Jelly for sex with condoms or masturbation. If you’re prone to vaginal yeast infections, choose a brand that’s glycerin-free. Silicone-based lubricants like Eros may be used with both condoms and latex sex toys (not silicone sex toys since they can ruin the material). But they’re tough to rinse off, may cause vaginal irritation for some, and can taste strange.
Petroleum oil-based lubricants (baby oil, Vaseline, etc.) and vegetable oils should be used for external masturbation and massage only. Never use them internally or with condoms, as they can cause latex to deteriorate, which can make condoms break. They also leave behind a residue in which germs can easily grow.
What might also help? If possible, have more sex. It increases healthy blood flow to your vulva and vagina, encouraging natural lubrication.

Consider Vaginal Moisturizer
"I also wish more women knew about vaginal moisturizers, which are different than lubricants," says Mintah. "Moisturizers are applied the same way, but they do get absorbed into the vaginal and vulvar tissues. They’re meant to be used regularly, not just during sex, and are effective at reducing itching and irritation."
Vaginal moisturizers can be found in the pharmacy and include brands like Replens and Vagisil. Make sure to read the application directions carefully and consider wearing a pad or panty liner since your vagina will release any product it doesn’t absorb.

You may feel dizzy or have mood swings
Symptoms of menopause can include lightheadedness and dizziness, which can also be signs of other health conditions. Ask your OBGYN about other possible causes like dehydration, low blood sugar, low blood pressure, anxiety or a heart condition if you experience this symptom often.
Mood swings can also accompany menopause. Mood changes can be related to fluctuating hormones. During the transition to menopause, called perimenopause, your ovaries start producing estrogen irregularly. Because estrogen helps to regulate brain chemicals like serotonin, which controls mood, fluctuating estrogen levels can affect your mood.
Changes in hormone levels can also affect your sleep and contribute to mood swings. The good news: Your emotions should eventually level out after you’ve reached menopause.

Menopause can affect your thinking and memory
Foggy thinking is another common symptom of menopause.
"Many women describe problems with mild memory loss and difficulty concentrating," says Mintah. Tasks involving working memory—the ability to take in new information, process it, and use it to make decisions—may feel especially challenging.
"Estrogen is thought to be important to cognitive function and the decrease in estrogen may be associated with these symptoms," she explains. Difficulty sleeping adds to the fog.
Sound familiar? If so, try this: Repeat new information like names, numbers, or instructions out loud when you hear them. Writing the information down may also help you remember it. A full night’s rest is also a proven brain booster, too.

Your depression risk goes up
“There’s an increased risk of depression in women during the menopausal transition, compared to their younger years,” says Mintah. “But this risk is generally thought to decrease in the early post-menopausal years,” she adds.
In general, women have double the lifetime risk of depression, compared to men. This is due, in part, to hormone changes that come with life stages like puberty, pregnancy, and menopause. When estrogen drops during menopause, specifically, it can interfere with your brain’s ability to regulate mood chemicals like serotonin.
Social pressures, family responsibilities, and gender inequalities also influence depression risk. During middle-age, it’s typical to juggle career, childcare, eldercare, financial and household responsibilities, contributing to burnout and depression among caregivers. If you experience signs of depression, such as persistent sadness, fatigue, or loss of interest in activities you usually enjoy, reach out to a mental health professional for help.

Hair May Grow In Unexpected Places
During menopause, hair can fade from areas like your head and grow in other places, such as your face and back. Unlike male-pattern balding which tends to occur in patches, menopause can cause overall thinning of hair related to decreasing estrogen and progesterone levels.
At the same time, certain types of androgen—the hormone responsible for male sex traits—might rise during perimenopause. This spike may not be dramatic, but since estrogen is lower at this point, it can be enough to promote male-pattern hair growth. Hormone changes might also result in acne, decreased skin elasticity, and thin, brittle nails.
"Collagen is what gives your tissues elasticity and keeps the skin and hair young-looking," explains Mintah. "The collagen content in your skin decreases when estrogens are low, leading to wrinkles and an aged appearance."

Abnormal Uterine Bleeding Can Happen
Abnormal uterine bleeding (AUB) can be an early sign of perimenopause, or start after months of not menstruating. Some people may lose up to 80 ml (1/3 cup) of blood in one cycle, bleed for over seven days at a time, or experience symptoms like weakness which may be related to blood loss and interfere with daily life. People who are obese or have uterine fibroids are more likely to experience AUB.
If you experience these symptoms, make an appointment with your OBGYN to get checked. Your HCP may recommend taking an iron supplement to treat anemia or using hormone therapy to reduce the bleeding. Depending on your blood work, symptoms, and medical history, they may also have you undergo additional tests to rule out other conditions like uterine fibroids.

Ask about your heart health
"Over the long term, estrogen deficiency can lead to an increased risk of heart disease," says Mintah. "This is thought to be due, in part, to changes in cardiovascular risk factors, such as cholesterol levels, which begin to change during perimenopause."
While menopause doesn’t cause heart disease, blood pressure, and cholesterol levels tend to increase during this time, even if you’re following the same healthy diet you always have and are getting regular exercise. These factors raise your risk of heart issues, so it’s important to have a conversation about screenings and prevention with your HCP. Heart disease is the number one killer of men and women in the United States.
You can start by discussing blood pressure and cholesterol checks with your HCP, as well as dietary changes, exercise, and stress management.

Mayo Clinic. Vaginal atrophy. May 2, 2019.
The North American Menopause Society. Changes in the Vagina and Vulva. Accessed December 8, 2020.
Centers for Disease Control and Prevention. HIV Risk Reduction Tool. Accessed November 9, 2020.
Bonnie Rothman Morris. Two Years After; Fighting Dryness, With Pills, Gels and Rings. The New York Times. June 6, 2004.
Vagifem. How Vagifem works in your body. Accessed November 9, 2020.
Johns Hopkins Medicine. Introduction to Menopause. Accessed November 9, 2020.
Cleveland Clinic. Can Menopause Cause Anxiety, Depression or Panic Attacks? November 25, 2019.
University of Rochester Medical Center. ‘Brain Fog’ of Menopause Confirmed. March 13, 2012.
Women’s Health Research Institute. Effect of Perimenopause on Cognition. 2014.
Harvard Gazette. Changes in memory tied to menopausal status. September 27, 2016.
BL Lasley, S Crawford, & DS McConnell. Adrenal androgens and the menopausal transition. Obstetrics and Gynecology Clinics of North America. September 1, 2012. 38(3), 467–475.
T Yasui, S Matsui, et al. Androgen in postmenopausal women. The Journal of Medical Investigation. 2012. 59(1-2):12-27.
HealthyWomen.org. Androgen. Accessed November 9, 2020.
Johns Hopkins Medicine. Menorrhagia. Accessed November 9, 2020.
BS Agpar, AH Kaufman, et al. Treatment of Menorrhagia. American Family Physician. June 15, 2007. 75(12):1813-1819.
Centre for Menstrual Cycle and Ovulation Research. For Healthcare Providers: Managing Menorrhagia Without Surgery. October 4, 2017.
Andrew M. Kaunitz. Menorrhagia During Perimenopause. Medscape. March 1, 2006.
JC Prior. Progesterone for Symptomatic Perimenopause Treatment - Progesterone politics, physiology and potential for perimenopause. Facts, Views & Vision in ObGyn. 2011, 3(2), 109–120.
American Heart Association. Menopause and Heart Disease. July 31, 2015.
University Health News Daily. Cholesterol Levels for Women May Increase After Menopause. April 20, 2020.
RA Lobo, SR Davis, et al. Prevention of diseases after menopause. Climacteric. June 4, 2014. Pages 540-556.
J Jin. Vaginal and Urinary Symptoms of Menopause. JAMA. 2017;317(13):1388.
MB Mac Bride, DJ Rhodes, & LT Shuster. Vulvovaginal atrophy. Mayo Clinic Proceedings. January 2010. 85(1), 87–94.
Cleveland Clinic. Do You Bleed After Sex? When to See a Doctor. September 1, 2017.
R Kagan, S Kellogg-Spadt, & SJ Parish. Practical Treatment Considerations in the Management of Genitourinary Syndrome of Menopause. Drugs & Aging, 36(10), 897–908.
Mayo Clinic. Estrogen (Vaginal route). October 1, 2020.
Medline Plus. Estrogen Vaginal. August 15, 2018.
J Patterson, L Millheiser, & ML Krychman. Moisturizers, Lubricants, and Vulvar Hygiene Products: Issues, Answers, and Clinical Implications. Female Sexual Dysfunction and Disorders. November 3, 2016. 8, pages213–221(2016).
Cleveland Clinic. Uterine Bleeding: Abnormal Uterine Bleeding. August 30, 2019.
Medscape. Abnormal (Dysfunctional) Uterine Bleeding Workup. December 7, 2018.
M Terauchi, T Odai, et al. Dizziness in peri- and postmenopausal women is associated with anxiety: a cross-sectional study. BioPsychoSocial Medicine. December 12, 2018. 12, 21.
National Sleep Foundation. Menopause & Sleep. Accessed December 7, 2020.
More On


video

slideshow


video


video
