More than 200,000 Americans are diagnosed with lung cancer annually. Every case is different, and certain treatments work better for some than for others. To better tailor therapy to each individual, oncologists may use biomarker testing, a diagnostic tool sometimes called genetic, genomic, molecular or mutation testing.
Biomarkers are measurable molecules found in the body’s tissues or fluids. They can indicate disease, changes in your biological processes—or that your body is functioning just fine. For patients with certain types of lung cancer, biomarker testing helps healthcare providers make a diagnosis, predict outcomes and response to various treatments, and monitor the disease during treatment.
Biomarker testing is constantly evolving, with many studies currently in progress. Here’s what you need to know right now.
How biomarker testing works
There are two main kinds of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). It’s estimated that between 80 to 85 percent of patients have NSCLC, the more common type, while 10 to 15 percent have SCLC. Biomarker testing can only be performed on people with NSCLC. It is not available to SCLC patients, though that may change in the future.
People with NSCLC often undergo this testing to reveal whether they would benefit from two newer types of cancer treatment, targeted therapy or immunotherapy—and if so, which medicines would best suit them.
- Immunotherapy uses drugs to help your immune system spot and wipe out cancer cells. Your levels of a protein called PD-L1 help determine if immunotherapy is right for you.
- Targeted therapy attacks specific molecules that promote the growth of cancer cells. This is different that standard chemotherapy drugs, which target all rapidly dividing cells in the body, both normal and cancerous. Biomarker testing can identify gene mutations that may respond to targeted therapy. EGFR, ALK, ROS1 and BRAF are all examples of mutations.
When specific treatment is better matched to the individual patient’s specific cancer, health outcomes often improve.
The basics of biomarker testing
Patients may undergo biomarker testing at or after diagnosis, or if NSCLC has recurred. Speak with your healthcare provider about your options. If you decide to go ahead, reach out to your health insurance provider to confirm you’re covered—or ask a member of your cancer care team to call, like your case manager or social worker.
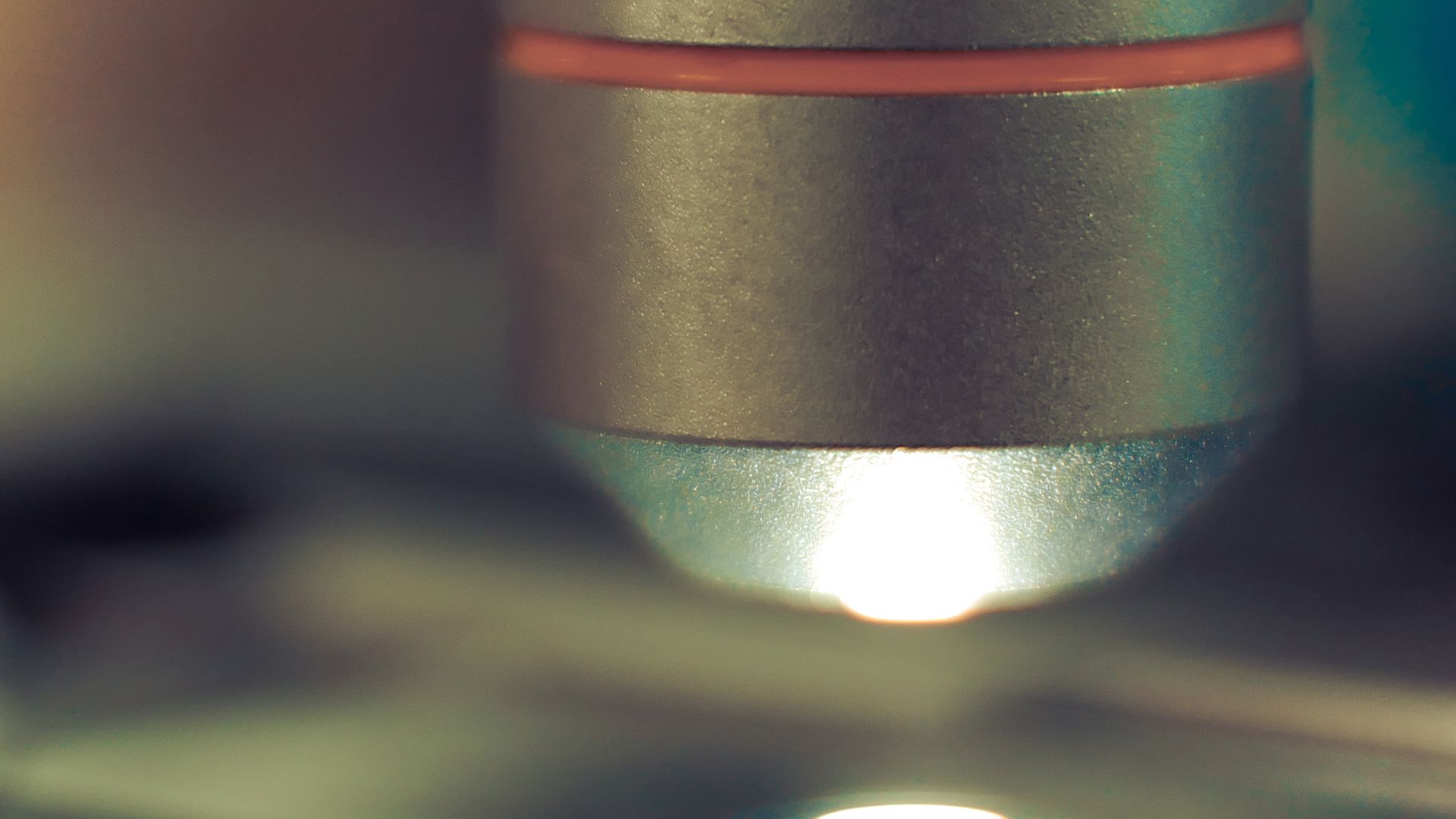
Here’s how testing is done: Your tumor will be biopsied or removed completely, and samples will be delivered to a lab for testing. Results should come back within two weeks, at which point an oncologist can interpret them and explain it to you. Blood or urine may also be tested for biomarkers—a technique called a “liquid biopsy.” This can help healthcare providers understand if a cancer has become resistant to a targeted therapy, and measure the response of a particular targeted therapy.
Those results will inform therapy recommendations moving forward—but they won’t be the only factors in your plan. Your general health, co-existing medical conditions, the type and stage of your cancer, and your treatment goals will also influence your healthcare provider’s strategy. Together, they can help you achieve the best possible health outcome.