Updated on April 13, 2023
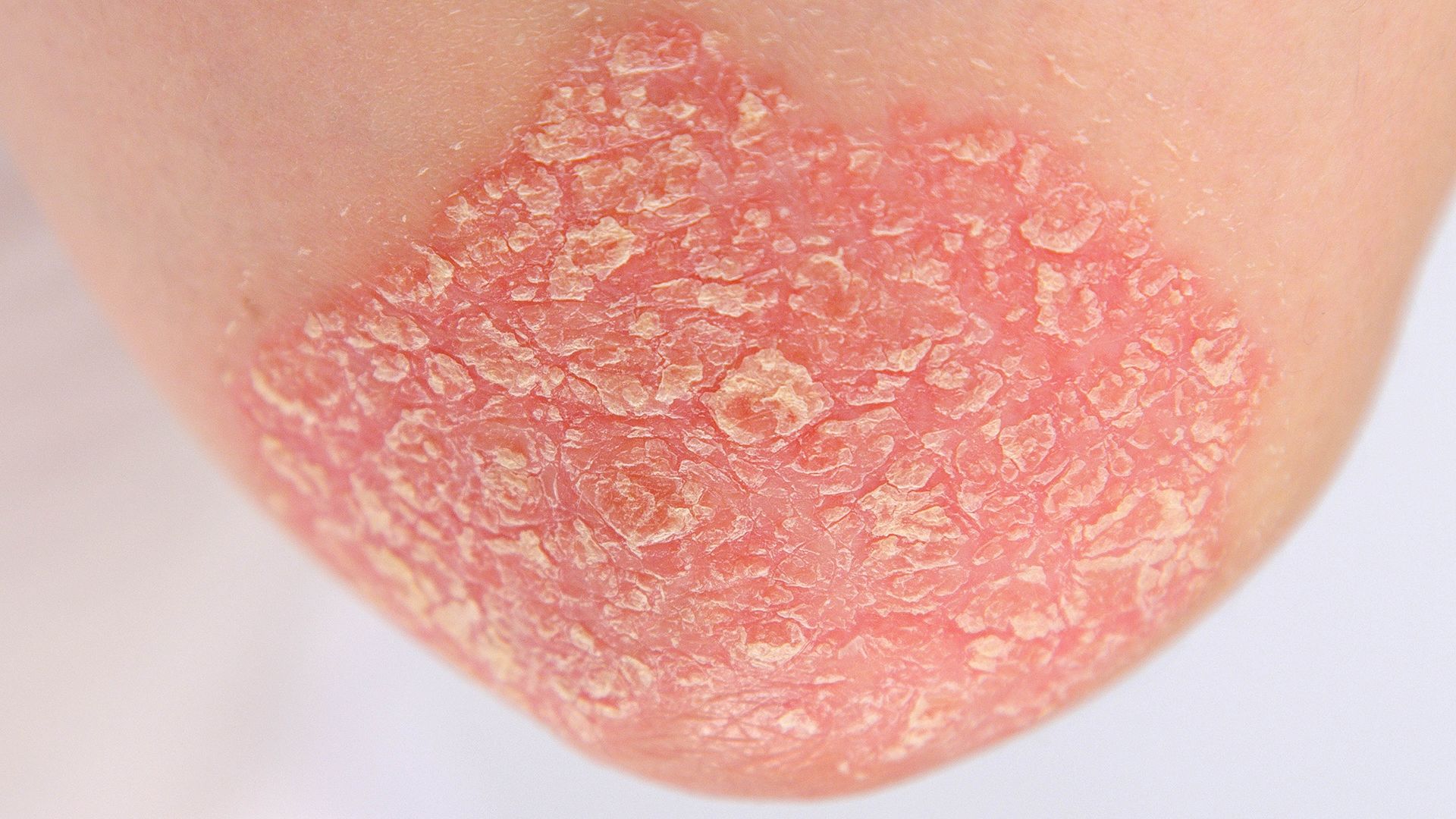
Psoriasis is an autoimmune condition that involves inflammation in the skin. It causes red or discolored, itchy, scaly patches of skin. People with psoriatic arthritis—a related condition—experience joint pain as well.
The reality is that psoriasis affects more than your skin or joints. The condition can also affect your mental health, your social life, and intimacy. People with psoriasis have a higher risk of depression than those who don’t have psoriasis, so it’s important to have a support network.
“For people with psoriasis, support groups can be helpful to discuss symptoms, treatments, and side effects with others going through it,” says Doris Day, MD, a dermatologist based in New York City. “Psoriasis is a pro-inflammatory condition that can affect other organs besides the skin.”
First, be sure you have the medical care you need. “It's important to have a multidisciplinary team—a dermatologist, internist, rheumatologist, cardiologist, and a gastrointestinal doctor as needed and depending on signs and symptoms,” Dr. Day says.
From there, it’s helpful to put in place the additional supports you’ll need on a day-to-day basis. Here’s how to get started.
Be honest with yourself
Sometimes the best support network starts with yourself. Living with a chronic disease like psoriasis can make life more challenging. It’s okay to admit that so you can begin to accept it. Then, you can start building a support system to help you manage it.
Invite your friends and family to learn about the disease
It can feel overwhelming to learn everything about psoriasis. Spread out the workload by inviting loved ones or friends to help you research it. Then share what you learn over lunch or coffee in a comfortable environment. This lessens then burden on you to know it all and helps those closest to you understand your condition and experience.
Day recommends that you have a loved one or friend attend medical appointments with you. That person can help take notes and be sure you’ve asked all questions you have. “It always helps to have a patient advocate at visits, and family members can be very helpful,” Day says.
Connect with a patient advocacy organization
The National Psoriasis Foundation (NPF) provides a wealth of resources to make managing your condition easier. Their website includes information about the condition, and their Patient Navigation Center can help patients find healthcare providers, learn about affordable treatments, prepare for appointments, and connect with others living with psoriasis.
Join a support community
The NPF’s One to One program matches you up with a volunteer living with psoriasis who is trained to provide one-on-one support and information. Children and teens living with psoriasis or psoriatic arthritis can check out NPF’s special section just for them.
The Psoriasis Community on Inspire has nearly 300,000 members who share and discuss a range of topics related to psoriasis management and treatment.
Join a meditation or activity group
Stress is a common trigger for psoriasis flare-ups and flare-ups can in turn lead to more stress. Mindfulness meditation and physical activity are effective stress reducers. Joining a meditation or exercise group makes it even easier to stick with a new routine.
You don’t have to join a gym either. The best physical activity is often whatever you enjoy and will keep doing. Maybe it’s joining a local volleyball team, trying yoga or tai chi, starting a walking group, or playing with your kids at the playground. It could be starting your dream garden or taking ballroom dance lessons with your partner. Just make it fun!
Consider finding a therapist or counselor
People living with psoriasis are at higher risk for depression. Research suggests that people with psoriasis may be more than 30 percent more likely to develop depression than those without psoriasis. At least 1 in 10 people with psoriasis has clinical depression, and nearly 3 in 10 experiences depression symptoms, according to some estimates.
Common symptoms of depression include fatigue, sleeping problems, the inability to enjoy things you once did, difficulty concentrating, and feeling hopeless or worthless. having less energy. If you’ve been experiencing any of these symptoms for two weeks or longer, consult with a healthcare provider. Depression is a real medical condition that requires treatment.
Ensure your intimate partner is supportive
Living with psoriasis might make intimacy feel more complicated, often because of self-consciousness. If you’re married or in a long-term relationship, be open with your partner about what living with psoriasis means for you and ways they can support you. If you’re dating, you will need to decide when it’s appropriate to talk to your partner. The sooner you discuss it, the sooner you will learn if they can offer the understanding and support you need.
Establish open communication with your employer as needed
Managing psoriasis often involves juggling multiple medical appointments, such as medication follow-ups, phototherapy treatments, or testing. Balancing work with your psoriasis management becomes easier when your supervisor knows what to expect. Plan a meeting with your boss when both of your stress levels aren’t high. Explain how your condition might influence your work, such as appointments you may have during work hours or accommodations you may need. For example, setting up an ergonomic workspace can help manage pain, and other strategies can make your job safer or more comfortable.
Managing a chronic condition can sometimes take a toll. Check in with yourself now and then to be sure you’re doing okay. If you aren’t, stress can worsen your psoriasis. Ask for help, whether it’s from a friend, a loved one, or a healthcare provider. The more support you have, the more easily you can successfully manage your psoriasis.